Imagine passing a bowel movement and feeling like a knife is slicing through your anus. The pain isn’t just sharp-it lingers for minutes, sometimes hours. You start avoiding the bathroom. You skip meals. You stop sitting down for long. This isn’t rare. It’s an anal fissure, and it’s more common than most people think.
What Exactly Is an Anal Fissure?
An anal fissure is a small tear in the lining of the anal canal, usually along the back wall (posterior midline). It’s not a cut from a sharp object-it’s a split caused by trauma, most often from passing hard or large stools. About 90% of fissures happen in the back, 10% in the front. The tear isn’t deep, but it hits sensitive nerves, which is why the pain is so intense. The body’s natural response makes it worse. When you feel pain during a bowel movement, your internal anal sphincter (a ring of muscle that controls stool passage) goes into spasm. This raises pressure in the area from a normal 15-20 mmHg to 25-30 mmHg. That spike cuts off blood flow to the tear by 40-60%. No blood flow means no healing. And without healing, the pain keeps coming. That’s the cycle: tear → pain → spasm → less blood → no healing → more pain.Why Do Fissures Happen?
Most anal fissures start with constipation. Straining to push out hard, dry stools stretches the anal lining until it tears. But it’s not just constipation. Diarrhea, childbirth, anal intercourse, and even inflammatory bowel diseases like Crohn’s can cause them. In babies, it’s often linked to formula or early solid foods. In adults, it’s usually diet-related. Here’s what the numbers say: 80-90% of acute fissures (those under 6-8 weeks) heal on their own. But if it lasts longer than eight weeks, it’s chronic-and that’s when the body’s healing system gives up. Chronic fissures develop a few telltale signs: a visible tear, a small skin tag near the anus (called a sentinel pile), and a swollen anal papilla inside. These aren’t just cosmetic-they’re signs the tear has been stuck in that pain-spasm cycle for too long.How Bad Is the Pain?
People describe it as a knife wound, a burning sensation, or a tearing feeling. It hits right when you poop-and it doesn’t stop. For 30 to 90 minutes after, the pain can radiate to your lower back, thighs, or even your genitals. One survey found 78% of patients felt this sharp, lingering pain. Nearly half said it made them cancel plans, skip work, or avoid sitting for days. The real problem? Many people don’t tell anyone. They’re embarrassed. They think it’s hemorrhoids. Or they assume it’ll go away. The average time between first symptoms and a correct diagnosis? Over 11 days. That’s more than a week of unnecessary pain because they didn’t know what they were dealing with.Conservative Treatment: The First Step
Before you think about surgery or strong meds, start simple. Most fissures heal with three things: fiber, water, and warmth.- Fiber: Aim for 25-30 grams a day. That’s 3 cups of cooked oats, a big bowl of lentils, a pear, and a handful of almonds. Don’t jump to 40g-that can make bloating worse. Too little fiber? That’s why 38% of conservative treatments fail.
- Water: Drink 2.5 to 3 liters daily. Fiber without water just makes stools bulkier and harder. Water turns fiber into a soft, spongy mass that passes easily.
- Sitz baths: Sit in warm (not hot) water for 10-15 minutes, 3-4 times a day, especially after pooping. It relaxes the sphincter, increases blood flow, and cleans the area. No fancy equipment needed-just a shallow basin or your bathtub.
Many people skip the sitz bath. They think wiping is enough. But cleaning with toilet paper alone irritates the tear. Warm water soothes it. It’s not optional-it’s essential.

Topical Medications: What Actually Works
If diet and baths don’t help in 2-3 weeks, it’s time for topical treatments. These aren’t miracle cures, but they break the cycle.- Nitroglycerin ointment (0.2-0.4%): Works in 45-68% of cases. But 20-32% of users get bad headaches. It relaxes the sphincter by releasing nitric oxide. Use it twice daily for 8 weeks.
- Diltiazem (2%) or nifedipine (0.3%): These calcium channel blockers are better tolerated. They heal 65-75% of fissures with fewer headaches. The Mayo Clinic now recommends these as first-line over nitroglycerin.
Applying them right matters. Use a finger (clean!) to put 1.25 inches of ointment inside the anus, 1 inch deep. Do it twice a day. Don’t just smear it on the outside. That’s why 29% of topical treatments fail-people don’t apply them correctly.
Botox Injections: A Middle Ground
If ointments don’t work, Botox is the next step. A doctor injects 15-30 units of botulinum toxin directly into the internal sphincter. It paralyzes the muscle for a few months, lowering pressure and letting the tear heal. Success rates? 50-80%. But here’s the catch: up to 40% of people see the fissure come back within a year. And it’s not cheap. It’s also not permanent. If it fails, you’re back to square one-or heading to surgery.Surgery: When Everything Else Fails
Sphincterotomy is the gold standard for chronic fissures. It’s a small procedure-15-20 minutes under local anesthesia. The surgeon makes a tiny cut in the internal sphincter to reduce pressure permanently. Healing rates? 92-98%. But there’s a trade-off. About 14% of patients develop minor fecal incontinence-usually just occasional gas or spotting. It’s not life-altering for most, but it’s a risk. That’s why doctors don’t jump to surgery. They wait. They try everything else first. Most people go back to work in 3.5 days. Full healing takes 6 weeks. No stitches. No hospital stay. Just rest, fiber, and patience.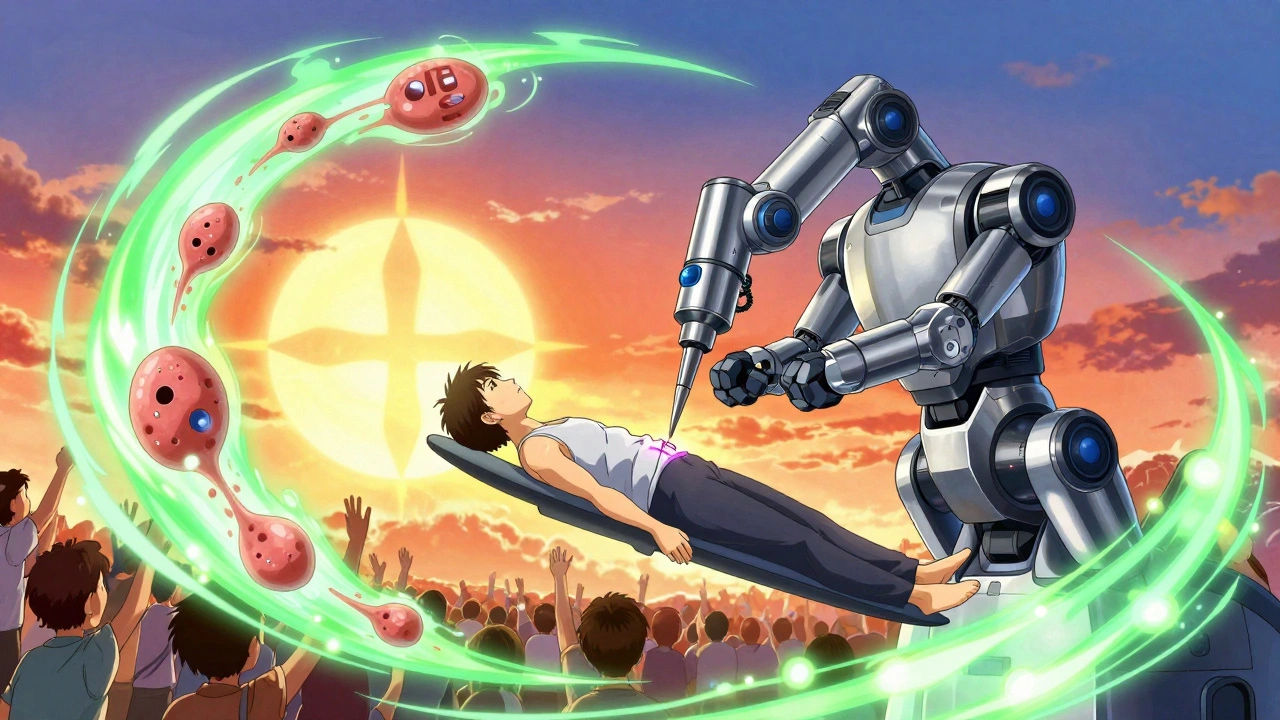
What Could Be Mistaken for a Fissure?
Not every anal pain is a fissure. Up to 10% of people diagnosed with one actually have something else: Crohn’s disease, anal cancer, or an abscess. If you’re under 30 and have no constipation history, or if you’re over 50 with unexplained weight loss, bleeding, or multiple fissures, you need further testing. A colonoscopy or anoscopy might be needed. Don’t assume it’s just a tear. Rule out the big stuff.What’s New in 2025?
Research is moving fast. In 2023, Johns Hopkins tested stem cell injections in 32 patients with stubborn fissures. After 8 weeks, 73% healed. It’s early, but promising. The European Society of Coloproctology updated its guidelines last year, putting diltiazem ointment at the top of the list for first-line treatment. Meanwhile, surgical rates are dropping. In 2010, 12% of fissure cases needed surgery. By 2023, that fell to 8%. Better meds mean fewer cuts. But there’s a warning: obesity and low-fiber diets are rising. Experts predict fissure cases could climb 15-20% over the next decade.What to Do Right Now
If you’re in pain today:- Stop straining. Use a footstool to raise your knees above your hips when you sit on the toilet. It aligns your colon and makes pooping easier.
- Start a high-fiber diet today. Add oatmeal, beans, chia seeds, apples with skin.
- Drink a full glass of water before every meal.
- Take a sitz bath after your next bowel movement. Just warm water. 15 minutes. No soap.
- If pain lasts more than 3 days, see a doctor. Don’t wait for it to get worse.
You don’t need to suffer. Fissures heal. But only if you break the cycle.
Been there. Thought it was hemorrhoids for weeks. Then I started sitz baths after every poop and swapped my bread for oatmeal. Pain cut in half by day 3. No joke. Warm water is magic.
Also, footstool. Get one. Your colon will thank you.
Ugh. I hate how doctors just say 'eat more fiber' like it's 1998. Nobody has time for that. And don't even get me started on nitroglycerin headaches. I'd rather just suffer.
Also, why is everyone so calm about this? It's literally torture.
Hey, I know it sounds basic but fiber + water + warmth really works if you stick with it. I had a chronic one for 11 months. Tried everything. Then I just did the 3 things the post said-no shortcuts. 6 weeks later, no pain. Not glamorous, but it’s real.
You got this. And you’re not alone in this weird, embarrassing club.
💛
Just tried the diltiazem cream. 2 days in. No headache. Felt like my butt finally gave me a hug. 🤗
Also, the footstool? Game changer. My dog now sits on it when I poop. He thinks it’s his throne.
Important note: if you’re over 50 and have unexplained bleeding or weight loss, don’t assume it’s a fissure. I had a misdiagnosis for 8 months. Turned out to be early-stage rectal cancer. Anoscopy saved my life. Please, get checked if things don’t improve in 2 weeks. This isn’t fearmongering-it’s fact.
Ugh, another ‘fiber is the answer’ post. Like we don’t all know that. The real issue is that our food system is broken. No one eats real food anymore. Processed crap + no water = anal carnage.
And don’t even get me started on how lazy doctors are. They’d rather prescribe a cream than fix the root cause. America’s healthcare is a joke.
Correction: the study cited from Johns Hopkins in 2023 had 32 patients, not 320. Also, stem cell therapy is still experimental-no peer-reviewed RCTs confirm long-term efficacy yet. Diltiazem remains first-line per 2024 ESCP guidelines. And yes, sitz baths should be 37-38°C, not hot. Details matter.
From India, here. We call this 'bhaiya ki dard'-brother’s pain. My uncle had one for years. He healed with aloe vera gel, warm coconut water, and sitting on a wooden stool. No meds. Just tradition + patience.
Also, if you’re in a hot climate, skip the soap. Just water. Trust me.
Why is this even a thing? We’re a developed country. Why are people still getting anal tears from constipation? Someone needs to ban processed snacks and soda. This is a public health failure.
And why do we whisper about it? It’s a medical condition. Not a sin.
You’re all wrong. The real solution is magnesium citrate. Every. Single. Time. Fiber doesn’t work if your body’s not absorbing water. I’ve had 3 fissures. Magnesium fixed all of them. No baths. No creams. Just 400mg at night. Done.
My mom had a fissure after having my little sister. She used witch hazel pads and sat in warm tea baths. Chamomile. Said it smelled like peace. She didn’t know about diltiazem or Botox. Just love and patience.
Also, if you’re scared to talk about it, just say ‘I’ve got a butt issue.’ People get it. No shame.