Statin Tolerance Calculator
Personalized Statin Risk Assessment
Based on SLCO1B1 genotype data from clinical studies. Results help guide statin selection to reduce muscle side effects.
Your Personalized Recommendation
If you’ve been told to take a statin but kept having muscle pain, you’re not alone. About 7 to 29% of people who take these cholesterol-lowering drugs report muscle-related side effects-cramps, weakness, or just a general feeling of being run down. For many, that’s enough to stop taking them, even if their doctor says it’s critical for heart health. But what if the problem isn’t your lifestyle, your age, or your dose? What if it’s your genes?
Why Some People Can’t Tolerate Statins
Statin drugs like simvastatin, atorvastatin, and rosuvastatin work by blocking an enzyme your liver uses to make cholesterol. That’s good for your arteries. But they also get pulled into muscle tissue by accident, and that’s where trouble starts. For most people, the body clears them safely. For others, something in their DNA makes it harder. That’s where the SLCO1B1 gene comes in. This gene makes a protein called OATP1B1, which acts like a ferry, shuttling statins from your blood into your liver. If your version of this gene has a specific mutation-called rs4149056, or the C variant-the ferry doesn’t work as well. That means more statin stays in your bloodstream, and more of it ends up in your muscles. The result? Higher risk of muscle damage. The data is clear: people with two copies of the C variant (CC genotype) have a 4.5 times higher risk of severe muscle injury when taking high-dose simvastatin compared to those with two normal copies (TT). Even one copy (TC) raises the risk by 2.6 times. About 15% of people of European descent carry one copy. Around 1 to 2% carry two. That’s not rare. It’s common enough to matter.Not All Statins Are Created Equal
Here’s the twist: this genetic risk doesn’t apply to all statins. The SLCO1B1 gene mainly affects simvastatin. It has little to no impact on atorvastatin or rosuvastatin. Why? Because those drugs use different pathways to get into the liver. That’s why clinical guidelines only recommend genetic testing before prescribing simvastatin-not the others. If you’ve had muscle pain on simvastatin, switching to pravastatin or fluvastatin might solve the problem. Studies show people with the high-risk CC genotype have 80% lower muscle side effects on pravastatin than on simvastatin. And pravastatin still lowers LDL cholesterol just as well. That’s not a compromise-it’s a smarter choice.What Other Genes Might Be Involved
SLCO1B1 is the star, but it’s not the whole cast. Other genes play supporting roles. CYP enzymes like CYP3A4 and CYP2D6 break down some statins. If you’re a slow metabolizer because of your genes, those drugs build up in your system. The ABCB1 and ABCG2 genes control how statins are pumped out of cells-flaws here can trap statins in muscle tissue. And newer research points to genes like GATM and CACNA1S, which affect muscle energy and calcium flow, possibly making muscles more vulnerable. Even more recently, a 2021 study found a gene called SOAT1 showed a strong statistical link to muscle symptoms, but no one yet knows exactly how it works. The science is still catching up. That’s why SLCO1B1 remains the only gene with clear, actionable guidelines.
Who Should Get Tested-and When
You don’t need to be tested before your first statin. But if you’ve had muscle pain on a statin before, testing makes sense. The American College of Cardiology says it’s reasonable to test before trying simvastatin again. The Clinical Pharmacogenetics Implementation Consortium (CPIC) goes further: if you’re CC genotype, avoid 80mg simvastatin entirely. Use a lower dose or switch. Some clinics now offer pre-emptive testing-testing your genes before any medication is prescribed. One study found that people who got tested upfront were 18.7% more likely to stick with their statin long-term. That’s huge. If you know your risk before you start, you can pick the right drug from day one.What the Test Actually Shows
The test is simple: a cheek swab or blood draw. Results come back in 5 to 10 days. You’ll get your genotype for SLCO1B1: TT, TC, or CC. If you’re TT, you’re low risk. TC? Moderate risk. CC? High risk-especially with simvastatin 80mg. But here’s the catch: SLCO1B1 only explains about 6% of all statin muscle symptoms. That means most people who have side effects don’t have this gene variant. Other factors matter too-age, kidney function, thyroid issues, interacting meds like fibrates or antibiotics, even vitamin D levels. Genetics isn’t the whole story. But it’s a big piece.Real People, Real Results
A 54-year-old woman in Minnesota stopped taking simvastatin after six months of unbearable leg cramps. Her doctor suggested stopping altogether. She didn’t want to. She got tested. Her SLCO1B1 result was CC. Her cardiologist switched her to pravastatin. Within three months, her muscle pain vanished. Her LDL dropped from 168 to 92. She’s been on it for over a year now. On the flip side, a man in Florida got tested after his third failed statin trial. His genes were normal. He still had pain. He eventually found out he was taking a statin with a drug interaction-he was also on a common antibiotic that blocked its breakdown. His genes weren’t the problem. His medication list was.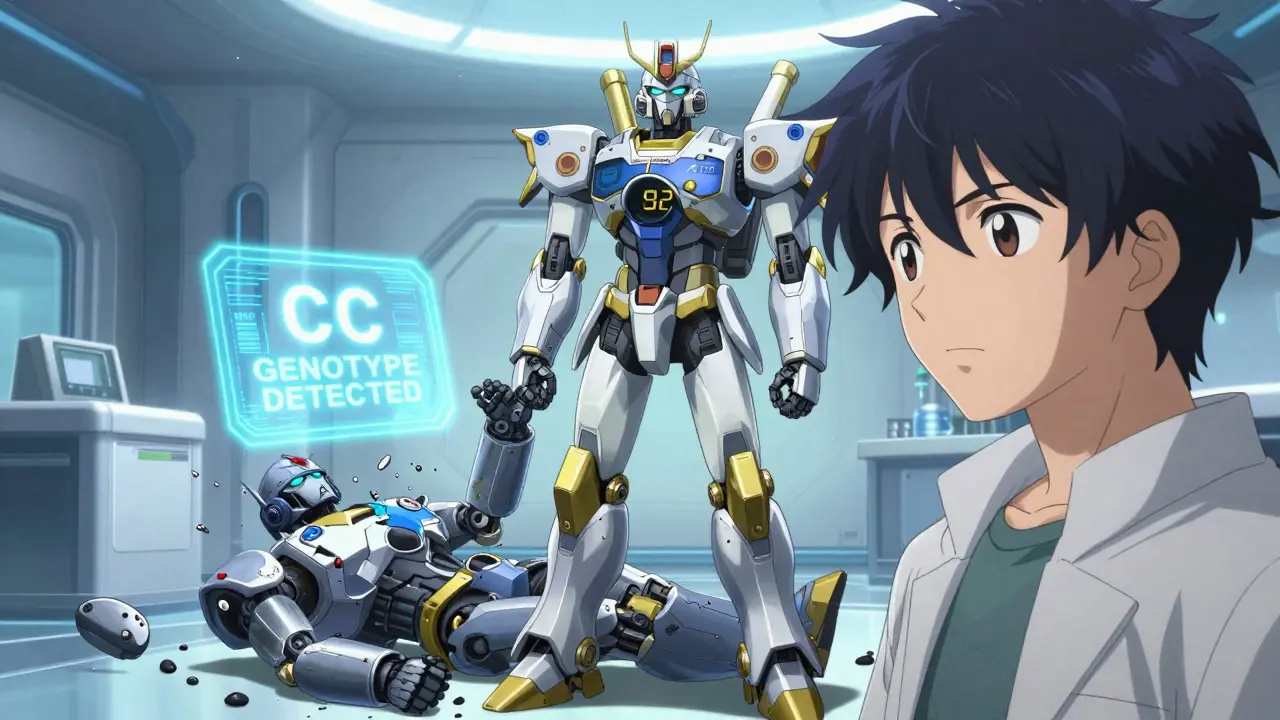
Barriers to Widespread Use
So why isn’t everyone getting tested? Cost and access. A standalone SLCO1B1 test runs $150 to $400 out-of-pocket. Insurance rarely covers it unless you’ve already had side effects. Only 28% of commercial insurers paid for it in 2022. Medicare doesn’t cover it at all unless it’s part of a broader genomic test program. Doctors aren’t always ready either. A 2021 survey found only 43% of primary care doctors felt confident interpreting the results. Cardiologists? 82%. That gap matters. If your doctor doesn’t know what to do with the result, the test doesn’t help. That’s changing. Big health systems like Mayo Clinic and Epic’s EHR now have built-in alerts. If you’re CC genotype and your doctor tries to prescribe simvastatin 80mg, the system pops up a warning. That’s progress.The Future: Beyond One Gene
The next step? Combining multiple genes into a single risk score. Early studies show that adding 15 other genetic variants to SLCO1B1 improves prediction accuracy-from 58% to 67%. That’s still not perfect, but it’s better. Researchers are also looking at how gene variants interact with lifestyle and other meds. The goal isn’t just to avoid side effects-it’s to personalize statin therapy so you get the most benefit with the least risk.What to Do If You’re Struggling with Statins
Don’t just quit. Talk to your doctor. Ask:- Could my muscle pain be related to my genes?
- Have I tried a different statin?
- Could I be on a dose that’s too high?
- Am I taking any other meds that might interact?
- Would a pharmacogenomics test help me make a better choice?
Is pharmacogenomic testing for statins covered by insurance?
Most insurance plans don’t cover standalone SLCO1B1 testing unless you’ve already experienced statin side effects. Medicare doesn’t cover it at all unless it’s part of a broader genomic testing program. Out-of-pocket costs range from $150 to $400. Some employer wellness programs or research studies may offer it for free.
Can I get tested without seeing a doctor?
Yes-companies like Color Genomics and OneOme offer direct-to-consumer pharmacogenomic tests. But these often include many genes and may not focus on statins specifically. Results can be hard to interpret without clinical support. It’s best to get testing ordered by a clinician who can connect the dots to your treatment plan.
Does SLCO1B1 testing work for all statins?
No. The SLCO1B1 gene variant strongly affects simvastatin and, to a lesser extent, lovastatin. It has little to no impact on atorvastatin, rosuvastatin, pravastatin, or fluvastatin. That’s why guidelines only recommend testing before using simvastatin, not other statins.
If my test shows I’m high risk, does that mean I can’t take statins at all?
No. It means you should avoid high-dose simvastatin (80mg). You can still take lower doses of simvastatin, or switch to a different statin like pravastatin or rosuvastatin, which are safer for your genotype. Most people with high-risk genes can still benefit from statin therapy-they just need the right drug.
How accurate is SLCO1B1 testing?
The test itself is highly accurate-it correctly identifies your genotype over 99% of the time. But the problem isn’t the test. It’s that SLCO1B1 only explains about 6% of statin muscle symptoms. Many people with side effects have normal results. Genetics is one tool, not a crystal ball.

Why are we wasting money on gene tests when we could just tell people to eat less junk and move more
Genetics is not an excuse for noncompliance. If you can't tolerate statins, you're not trying hard enough.
So let me get this straight - we're gonna test my DNA before I take a pill, but my doctor won't even ask if I'm taking ibuprofen every day or if I'm a couch potato who eats fries for breakfast? This whole thing feels like a scam to sell more tests. I'm not saying genes don't matter, but 6%? That's like blaming your car crash on the color of the road.
My uncle took simvastatin for 10 years, never had a problem. Then he started taking a generic antibiotic for a sinus infection and ended up in the ER with rhabdo. No gene test would've caught that. It's the combo, not the SNP.
And why are we acting like pravastatin is some magic bullet? It's weaker. My LDL only dropped 12 points on it. I'd rather take the risk than live with cholesterol that high.
Also, who wrote this? Some pharma rep? The tone's too clean. Like it was copy-pasted from a Medscape article. Where's the real talk? Where's the patient who got kicked off statins and still had a heart attack? That's the story nobody wants to tell.
ok but like… why is this even a thing? my doc just gave me a script and said ‘take this’ and now i’m supposed to get a dna test? i dont even know what my blood type is. also i think my neighbor’s dog has more health literacy than me
also why does every article about meds now need to be 12 paragraphs long? i just wanna know if i can still drink coffee
❤️ this is such an important topic!! I had muscle pain on simvastatin and thought I was just getting older… then I got tested and turned out to be CC. Switched to pravastatin and life changed. I can finally walk my dog without feeling like my legs are made of cement 😭
Also - if you’re reading this and scared to talk to your doctor? Just say: ‘Can we talk about pharmacogenomics?’ Most docs will look it up. I promise. You deserve to feel good while staying healthy.
And if you’re worried about cost - ask if your hospital has a research study. I got mine free through my clinic’s genomics program. No one asked me for money.
Thanks for sharing this. I’ve seen too many patients quit statins because they were scared or frustrated, and then end up with a heart attack they could’ve avoided. Genetics isn’t the whole story, but it’s a powerful tool - especially when you’ve already had a bad reaction.
I work in primary care. We don’t test everyone, but we do test after one failed statin. It’s not expensive compared to an ER visit or stent. And honestly? It’s the most respectful way to treat someone - not just as a number, but as a person with a unique biology.
Oh wow, so now we’re blaming the gene for your laziness? Congrats, science has finally found a way to make you feel worse about not exercising.
Let me guess - next they’ll test your DNA to see if you’re genetically predisposed to not liking kale.
My grandma took simvastatin for 20 years, never had a problem. She also walked 5 miles a day and never ate processed food. Coincidence? Maybe. But I think your genes are just an easy excuse for bad habits.
Hi everyone - I just want to say this thread is actually really helpful. I’ve been scared to bring up genetics with my doctor because I thought they’d think I was crazy.
But after reading this, I’m going to ask for the test next week. I’ve had muscle pain on two different statins and I’m tired of being told it’s ‘all in my head.’
If you’ve been through this - you’re not alone. And asking for help isn’t weakness. It’s advocacy.
USA always think they can fix everything with science. In Nigeria we just eat plantain and walk. No gene test needed. Your body tells you what to do. You just too lazy to listen. This statin thing is western problem. You eat too much meat and sit too much. Simple.
SLCO1B1 explains 6 percent of cases so why are we making a big deal about it