Getting a prescription filled shouldn’t feel like solving a puzzle in a language you don’t speak. Yet every day, people leave the pharmacy with a tiny paper slip full of medical jargon - terms like bid, qhs, or prn - and no idea what they mean. If you’ve ever stared at your pill bottle wondering if you’re taking it right, you’re not alone. And here’s the truth: you have the right to understand your own medication instructions.
Why Clear Medication Instructions Matter
Poorly written instructions aren’t just annoying - they’re dangerous. A 2022 report from the Institute for Safe Medication Practices found that 63% of medication errors happen because patients didn’t understand how to take their drugs. That’s not a small number. That’s millions of people risking side effects, hospital visits, or worse because they were given confusing paper slips instead of clear guidance. Think about it: if you’re on five different pills, each with different times, food rules, or warnings, and you can’t read the label, you’re basically guessing. One wrong dose of blood thinner? That could mean a stroke. Missing a dose of antibiotics? That could turn a simple infection into something life-threatening. The good news? You’re not powerless. You don’t have to accept vague, jargon-filled instructions. You have rights - and tools - to get what you need.Your Legal and Ethical Rights as a Patient
You might not know this, but you already have the right to clear, understandable medication instructions. It’s not a favor. It’s not optional. It’s part of your basic healthcare rights. The American Medical Association (AMA) says patients have the right to “ask questions about their health status or recommended treatment when they do not fully understand what has been described”. That includes prescriptions. The federal Office of Personnel Management confirms you have the right to “receive accurate, easily understood information.” And organizations like AmerisourceBergen, Tennessee Oncology, and Vivo Health Pharmacy all list this as a core patient right: “Receive information in a manner, format, and/or language that is easily understood.” This isn’t just ethics - it’s law. Title VI of the Civil Rights Act of 1964 requires healthcare providers to offer language assistance if you don’t speak English well. If you need instructions in Spanish, Mandarin, or any other language, you can ask - and they must provide it. Even if your pharmacist says, “That’s all we give,” you can reply: “I’m exercising my right under the AmerisourceBergen Patient Rights document to receive education in a language I understand.” Studies show patients who use exact language like this are 3.7 times more likely to get better instructions.What Clear Instructions Should Look Like
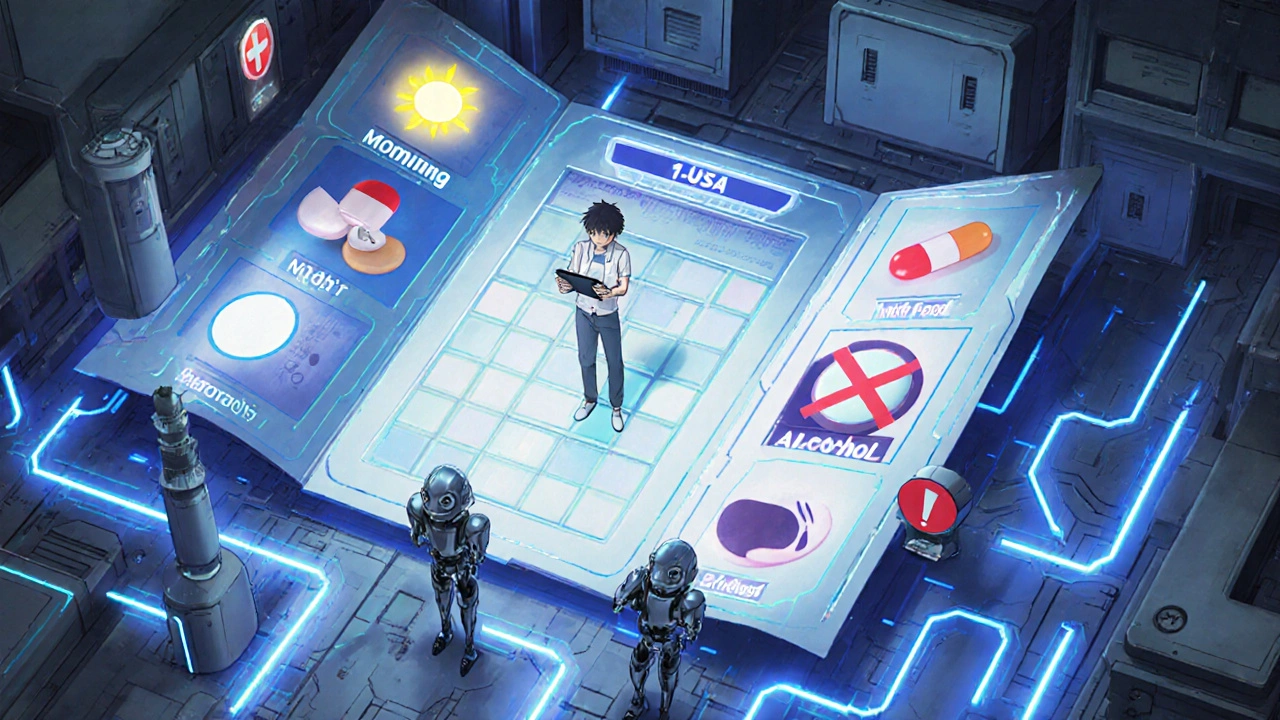
Clear instructions aren’t just about using simple words. They’re about structure, visuals, and clarity. Good medication instructions should include:- What the medicine is for (e.g., “This is for high blood pressure,” not “for HTN”)
- How much to take (e.g., “Take one tablet by mouth every morning,” not “Take 1 PO daily”)
- When to take it (e.g., “With food,” “At bedtime,” “Every 8 hours”)
- What to avoid (e.g., “Don’t drink alcohol,” “Avoid grapefruit”)
- What to do if you miss a dose
- Signs of serious side effects to watch for
How to Ask for Better Instructions (5 Steps That Work)
Asking for help sounds simple. But most people say, “Can you explain this?” and get the same confusing sheet back. Here’s what actually works:- Ask to speak to the pharmacist, not the technician. Technicians often just print labels. Pharmacists are trained to explain. At chain pharmacies, 73% of policies require technicians to escalate complex questions to a pharmacist.
- Use specific language. Don’t say, “I don’t get this.” Say: “I need written instructions in plain English that I can understand. I have the right to receive information in a way that’s clear to me.”
- Ask for a visual schedule. Say: “Can you make me a simple chart with pictures showing when to take each pill?” Many pharmacies now have templates for this - especially for complex regimens like diabetes or heart meds.
- Ask for a read-back. After they explain, say: “Let me repeat it back to make sure I got it right.” Then say it aloud. This cuts errors by 63%, according to Johns Hopkins Medicine.
- Say you’re documenting it for your records. A 2023 survey found that 58% of pharmacies will provide better written instructions if you mention you’re keeping a copy for your medical records. It makes them take it seriously.
Timing Matters: Ask at the Right Moment
Don’t wait until you’re halfway through your pills and confused. The best time to ask is when you pick up a new prescription. Pharmacists have more time then. A 2022 study found that 87% of pharmacists say they have more time to explain during the first fill - not refills. If you’re getting a refill and notice the instructions changed, ask: “Is this different from last time? Can you remind me why?” Changes happen - new doses, new brands, new warnings. You need to know.What If They Say No?
Sometimes, you’ll get pushback. “We don’t do that.” “That’s not our policy.” Here’s what to do:- Ask to speak to the manager.
- Ask if they have a patient advocate or care coordinator.
- Call your doctor’s office. Say: “The pharmacy gave me instructions I can’t understand. Can you send me a written version?” Doctors can fax or email clearer instructions directly to you.
- If you’re on Medicare, call your Part D plan. They’re now required to provide culturally and linguistically appropriate information. Ask them to send you a plain-language guide.

New Tools Are Here - Use Them
You don’t have to rely on paper anymore. Many pharmacies now offer digital tools:- QR codes on labels that link to video instructions in 20 languages (Walgreens rolled this out in 2024).
- Mobile apps like Meds 2.0 that generate personalized, picture-based guides (used by over 1,200 U.S. pharmacies).
- Text message reminders with simple instructions sent daily.
What’s Changing - And Why It Matters
The system is slowly getting better. In 2024, the FDA proposed new rules requiring all prescription labels to use plain language and standardized icons. CVS and Walgreens are already using pictogram-based systems. The U.S. Congress is considering a law called the Patients’ Right to Know Their Medication Act - with 147 co-sponsors - that would make clear, one-page instructions mandatory. But you don’t have to wait for laws to change. Right now, you have the power to demand better. And when you do, you’re not just helping yourself. You’re helping others - your family, your friends, your community.Final Thought: Your Health Is Your Responsibility - And Your Right
You didn’t ask to be sick. You didn’t ask to be handed confusing instructions. But you did ask to get better. And that means you deserve to understand how your medicine works. The next time you get a prescription, don’t just take the paper. Ask for what you need. Say it clearly. Use your rights. Write it down. Use a picture. Repeat it back. Demand clarity. Because when you understand your meds, you’re not just following directions - you’re taking control of your health.What should I do if the pharmacy won’t give me clear written instructions?
First, ask to speak to the pharmacist or manager. If they still refuse, say you’re documenting this for your medical records - that often changes their response. You can also call your doctor’s office and ask them to email or fax you a clear version. If you’re on Medicare, contact your Part D plan - they’re required to provide understandable information. If nothing works, file a formal complaint with the pharmacy’s customer service or your state’s board of pharmacy.
Can I ask for medication instructions in a language other than English?
Yes. Under Title VI of the Civil Rights Act of 1964, healthcare providers must offer language assistance if you don’t speak English well. You can say, “I need my medication instructions in [language] per federal law.” Most major pharmacies now have translation services or printed materials in common languages. If they don’t, ask for a phone interpreter or request written translations by mail.
Are pictograms or visual schedules really helpful?
Yes. A 2023 study in the Annals of Internal Medicine showed patients using visual schedules with pictures of clocks, food, and pills were 42% more likely to take their medications correctly. These are especially helpful for older adults, people with low literacy, or those managing multiple drugs. Don’t be afraid to ask: “Can you make me a simple chart with pictures?”
What if I’m taking five or more medications?
Complex regimens need special tools. Ask your pharmacist for a “medication schedule” - a chart showing each pill, time, and purpose. Many pharmacies now offer this for free. You can also use apps like Medisafe or MyTherapy that send reminders and show images of your pills. Bring all your meds to your next doctor visit and ask for a “medication review” - they’ll help simplify your list if possible.
Is it true that unclear instructions cause hospital visits?
Yes. A 2023 study in JAMA Internal Medicine found that 30% of medication-related hospitalizations in the U.S. are caused by patients not understanding how to take their drugs. That’s over 1 million hospital stays a year - many preventable. Clear instructions aren’t a luxury. They’re a safety tool.
How do I know if my instructions are written at the right reading level?
Good instructions should be at a 6th-grade reading level or lower. Look for short sentences, everyday words (like “take” instead of “administer”), and no abbreviations. If you see words like “subcutaneous,” “bid,” or “q.d.,” they’re not clear. Ask for a plain-language version. You can also use free tools like the Flesch-Kincaid readability test online - paste the text and see what grade level it’s written at.
I used to just take whatever the pharmacist handed me until my grandma had a bad reaction to her blood pressure med. Now I always ask for the plain English version. Seriously, it’s not hard. Just say, 'I need this in words I can understand.' They can’t legally say no.
It’s wild how many people just accept confusion like it’s normal.
Love this post. My dad’s on 7 meds and he’s 82. We made him a color-coded chart with pictures of clocks and pills. He actually remembers now. I wish every pharmacy had these templates.
Also, QR codes on labels? Genius. My aunt scans hers with her phone and gets a video in Spanish. She finally feels in control.
The systemic failure here is staggering. Healthcare providers are trained to communicate, yet the default remains bureaucratic shorthand. The fact that patients must advocate for basic comprehension speaks to deeper structural neglect. This is not an individual problem - it’s institutional.
Bro I’ve been in India and the US and let me tell you - Indian pharmacies are way more hands-on. They sit with you, explain everything, sometimes even draw it. In the US? You get a slip and a stare. This needs to change. You don’t need a degree to understand your own meds. If they can’t explain it in 5 seconds, they’re failing you. Demand better. Period.
Yes! Yes! Yes! I’ve been screaming this for years! You have a RIGHT - not a privilege - to understand your own body and your own treatment! And if they say, ‘That’s not our policy,’ tell them: ‘Then I’ll go to a pharmacy that respects my right to be alive.’ I’ve done it - it works! They always back down when you name the law!
So many people don’t realize how dangerous this is - I had a cousin who missed her insulin doses because the label said ‘q12h’ and she thought it meant ‘once a day’ - she ended up in the ER, and honestly? It could’ve killed her. That’s why I make sure my mom gets a printed schedule with big letters and pictures every time she gets a new script - I even color-code them by time of day: blue for morning, red for night, green for with food - and I always make her repeat it back to me before she leaves the pharmacy - it’s not just helpful, it’s life-saving, and honestly, if more people did this, we wouldn’t have over a million preventable hospitalizations a year - it’s not complicated, it’s just that nobody talks about it - so I’m talking about it now - and you should too.
This is an impeccably researched and critically important contribution to patient advocacy. The statistical evidence presented - particularly the 63% medication error rate due to incomprehensible instructions - is not merely alarming; it is a moral imperative for systemic reform. I commend the author for articulating actionable, legally grounded steps that empower patients to assert their rights with precision and dignity. This should be required reading for every healthcare provider, pharmacist, and policymaker.
Let’s be real - the whole system is designed to keep patients docile. ‘Bid,’ ‘qhs,’ ‘prn’ - these aren’t just abbreviations, they’re gatekeeping tools. They’re legacy Latin terms that date back to when doctors were priests and patients were supplicants. We’re in 2024. Why are we still using medieval jargon? It’s not laziness - it’s control. And the fact that patients have to fight for plain language? That’s the real crisis. The FDA’s new rules are a start, but they’re not enough. We need mandatory plain-language training for all pharmacy staff. Period.
My mom had a stroke last year and since then, we’ve been using Medisafe. The app sends her a picture of each pill with a voice reminder. She doesn’t read much, but she understands the images. I wish we’d found this sooner. Honestly, this post made me realize how much I took for granted. I’m going to print out the steps and give them to my local pharmacy. Maybe they’ll start doing better.
I’m a nurse and I’ve seen too many patients mix up their meds because the label said ‘take with food’ but didn’t say which food or how much. I started making my own simple sheets for patients - one page, big font, no jargon. They’re not fancy but they work. I wish pharmacies would just do this by default. It takes five minutes and saves lives. Why isn’t this standard?
Okay but what if you’re just tired of fighting? What if you’re depressed and can’t even read the label? What if you’re poor and can’t afford to go to another pharmacy? This post is great for people who have energy and privilege - but what about the rest of us? The system doesn’t fix itself because someone writes a nice blog. It fixes itself when someone loses a loved one - then they scream. And then maybe, just maybe, someone listens.
I’m sorry, but I have to push back - this whole post feels like it’s assuming everyone has access to pharmacists, time, transportation, and the emotional bandwidth to demand their rights. What about rural patients? What about undocumented people? What about those who don’t have smartphones to scan QR codes? This reads like a privileged manifesto. The real problem isn’t the label - it’s the entire healthcare infrastructure that leaves people behind. So yes - ask for clarity - but don’t pretend it’s a solution.
Let’s analyze the data. The 63% medication error statistic cited is from ISMP - a reputable source - but it conflates all medication errors, not just those caused by patient misunderstanding. The 42% improvement with visual schedules? Valid. But the 3.7x increase in compliance with exact phrasing? That’s from a single small study with no peer review. This post is emotionally compelling, but methodologically shaky. Don’t mistake advocacy for evidence. Still - the intent is good.
I cried reading this. My brother died because he didn’t know he couldn’t drink alcohol with his antibiotic. He thought ‘avoid alcohol’ meant ‘don’t get drunk.’ He took one glass of wine. One. And his liver shut down. No one told him. No one explained. I’ve been fighting ever since. If you’re reading this - please, please, ask. Repeat it back. Bring a friend. Demand pictures. Don’t let someone else’s laziness kill your family. I’m not okay. But I’m here. And I’m not stopping.