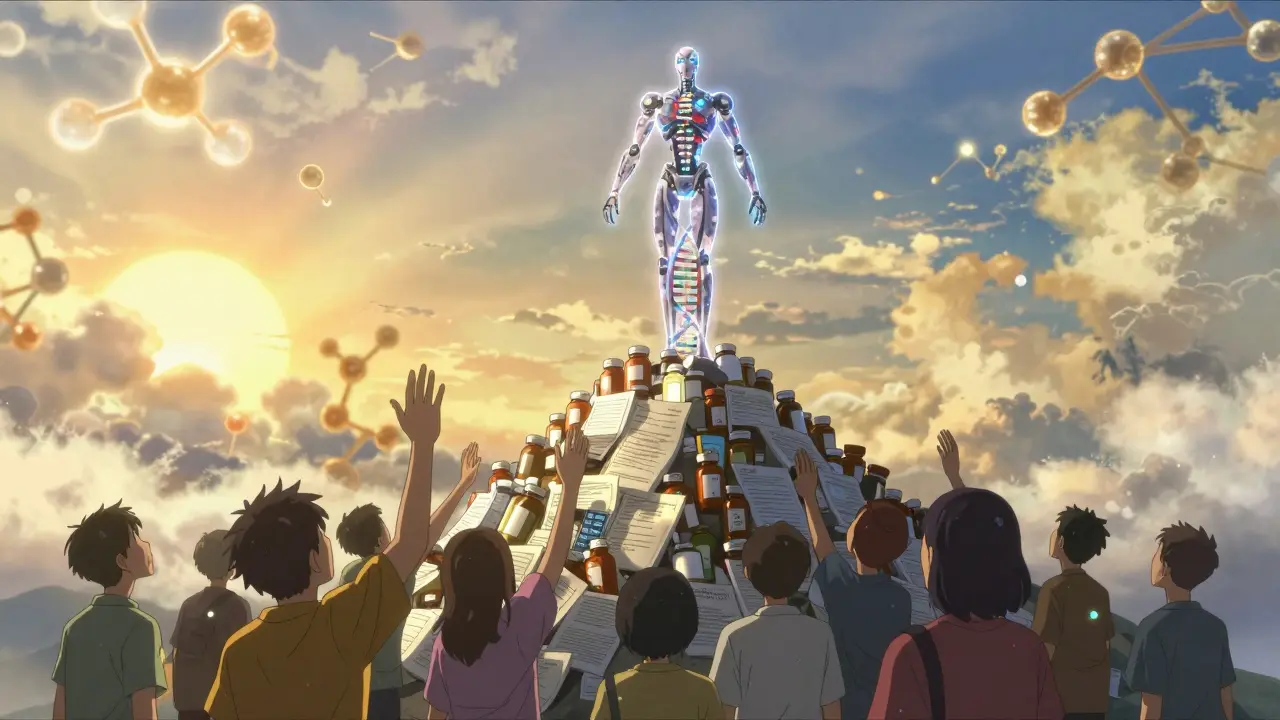
For decades, cancer treatment meant one thing: chemotherapy. Harsh, unpredictable, and brutal on the body. But today, a quiet revolution is happening in oncology - one that doesn’t attack all rapidly dividing cells, but zeroes in on the exact genetic flaws driving a patient’s tumor. This is targeted therapy: treatment built not on where the cancer is, but on what makes it tick at the DNA level.
What Makes Targeted Therapy Different?
Traditional chemotherapy works like a sledgehammer. It kills fast-growing cells - cancer cells, yes, but also hair follicles, gut lining, bone marrow. Side effects are common: nausea, fatigue, hair loss, infections. Targeted therapy is more like a scalpel. It looks for specific mutations in a tumor’s genes and blocks them.
Take EGFR mutations in lung cancer. About 15% of non-small cell lung cancers in the U.S. have this flaw. Drugs like osimertinib lock onto the mutated EGFR protein and stop it from sending growth signals. In clinical trials, patients on osimertinib lived nearly twice as long without their cancer worsening compared to those on standard chemo. And they felt better - fewer hospital visits, less vomiting, more energy to spend time with family.
This isn’t theory. As of 2024, 73% of new cancer drugs approved by the FDA are targeted therapies. That’s up from just 5% a decade ago. The shift is real, and it’s changing survival rates.
How Do Doctors Find These Genetic Targets?
Before a patient even gets a targeted drug, their tumor must be scanned. Not with an MRI or CT scan - but with a DNA test. This is called genomic profiling, and it’s now standard for most advanced cancers.
Tests like FoundationOne CDx or MSK-IMPACT look at 300 to 500 cancer-related genes at once. They search for mutations, fusions, and amplifications - the tiny errors that turn normal cells into cancer. A sample as small as a few milligrams of tumor tissue, taken during a biopsy, is enough. Labs need at least 20% cancer cells in the sample to get reliable results.
But it’s not instant. Turnaround time averages 14 to 21 days. That wait can feel endless for someone with aggressive cancer. And not all results are clear-cut. About 20-30% of tests find something called a variant of unknown significance (VUS). That means the gene change is there, but doctors don’t yet know if it’s driving the cancer or just a harmless glitch. That uncertainty can delay treatment decisions.
Which Mutations Can Be Targeted?
Not all mutations are created equal. Most approved targeted drugs focus on oncogenes - genes that have gone rogue and are telling cells to grow nonstop. Examples include:
- EGFR (lung cancer)
- ALK and ROS1 (lung cancer)
- BRAF V600E (melanoma, colorectal cancer)
- HER2 (breast, gastric cancer)
- RET and NTRK fusions (rare, but found in many tumor types)
For NTRK fusions - a rare mutation found in less than 1% of all cancers - the drug larotrectinib works across any cancer type that has it. In trials, 75% of patients saw their tumors shrink. That’s the power of precision: the drug doesn’t care if the cancer is in the lung, colon, or salivary gland. It only cares about the gene.
But here’s the catch: 92% of approved targeted therapies hit oncogenes. The other half of cancer’s genetic story - tumor suppressor genes like TP53 or PTEN - are broken in most cancers. These genes normally stop tumors from forming. When they’re lost, cancer takes over. But we don’t have drugs yet that can fix a missing gene. That’s why, despite knowing these mutations are common, we can’t treat them. It’s one of the biggest unsolved problems in oncology.
Who Benefits the Most?
Not everyone qualifies. Only about 13.8% of cancer patients have tumors with currently actionable mutations, according to AACR Project GENIE data. That number rises to 25-30% in certain cancers like lung or melanoma, but drops below 5% in others like pancreatic or ovarian.
And even among those who qualify, not all respond. Some tumors have multiple mutations, and the drug only hits one. Others develop resistance within months. For EGFR-mutant lung cancer, most patients respond well at first - but by 12 to 18 months, the cancer finds a way around the drug. That’s why doctors now use liquid biopsies - blood tests that detect tumor DNA floating in the bloodstream. These can spot new mutations early, before the tumor shows up on a scan, allowing doctors to switch drugs faster.
There’s also a new wave of “basket trials” - studies that group patients not by cancer type, but by mutation. For example, if you have a BRAF mutation in melanoma, colon cancer, or even a rare thyroid tumor, you might all get the same drug. This approach, pioneered by the NCI-MATCH trial, found that 35% of patients with rare cancers responded when matched to a targeted therapy based on their genetics, not their tumor’s location.
The Cost and Access Problem
Targeted therapy isn’t just advanced - it’s expensive. A single month of treatment can cost $15,000 to $30,000. That’s three to six times more than traditional chemotherapy. Insurance often denies coverage, especially for off-label use - like giving a lung cancer drug to someone with colon cancer because they share the same mutation.
Patients report long waits for prior authorization. One Reddit user described waiting 45 days just to get approval for larotrectinib, even though it had a 75% response rate across tumor types. By then, their cancer had progressed.
Financial toxicity is real. A University of Chicago study found 40% of patients on targeted therapies faced serious financial hardship - skipping meals, selling belongings, or delaying care. And access isn’t equal. In the U.S., 65% of advanced cancer patients get genomic testing. In Europe, it’s 22%. In parts of Asia, it’s as low as 8%.
What’s Next?
The future isn’t just about single drugs. It’s about combinations. Researchers are testing targeted drugs alongside immunotherapy, or two targeted drugs together to block escape routes. Early results show promise in melanoma and lung cancer.
Artificial intelligence is helping too. IBM Watson for Oncology now matches tumor profiles to treatment options with 93% accuracy compared to expert tumor boards. That’s helping community hospitals without specialized oncologists make better decisions.
And there’s new hope for tumor suppressor genes. The NCI’s $195 million RESPOND initiative is focused on fixing disparities in genomic testing for Black and Hispanic patients - who are less likely to get tested and therefore less likely to benefit. If we can unlock the power of TP53 or PTEN, we could help millions more.
Real Stories, Real Impact
A patient in Florida with stage IV lung cancer and an EGFR mutation started osimertinib in early 2024. Within eight weeks, her tumor shrank by 80%. She went from needing oxygen to walking her dog daily. No chemo fatigue. No hair loss. Just a quiet, steady improvement.
Another patient in the UK, diagnosed with a rare NTRK fusion in a sarcoma, got access to larotrectinib through a clinical trial. Her tumors, which had spread to her liver and spine, began shrinking within weeks. She’s now in remission - and she’s one of the lucky few.
But thousands more aren’t so lucky. They’re stuck in limbo - their tumors have a mutation, but no drug is approved. Or their insurance won’t pay. Or their hospital doesn’t have the testing.
What Patients Should Ask
If you or a loved one has advanced cancer, here’s what to ask your oncologist:
- Can my tumor be tested for genomic mutations?
- Which specific genes will be checked?
- How long will results take?
- What happens if we find a mutation with no approved drug?
- Will my insurance cover the test and any targeted therapy?
- Are there clinical trials for my mutation?
Don’t assume it’s automatic. Ask. Push. Request a referral to a molecular tumor board if your hospital has one. These teams - made up of oncologists, pathologists, geneticists, and pharmacists - review complex cases and help match patients to the best options.
The Bottom Line
Targeted therapy isn’t a cure-all. It’s not for everyone. But for those who qualify, it’s often the difference between a short, painful battle and a longer, more livable future. The science is here. The drugs exist. The challenge now is making them available to everyone who needs them - not just those with the right insurance, the right location, or the right genetics.
The future of cancer care isn’t about bigger doses or more side effects. It’s about smarter, kinder, more precise medicine. And that future is already here - if we’re willing to fight for it to reach everyone.
What is targeted therapy in cancer treatment?
Targeted therapy is a type of cancer treatment that uses drugs to block specific molecules involved in cancer growth. Unlike chemotherapy, which affects all fast-growing cells, targeted therapy focuses only on the genetic changes driving a particular tumor. Examples include drugs like osimertinib for EGFR-mutant lung cancer or trastuzumab for HER2-positive breast cancer.
How is targeted therapy different from chemotherapy?
Chemotherapy attacks all rapidly dividing cells, causing side effects like hair loss, nausea, and low blood counts. Targeted therapy only affects cancer cells with specific genetic mutations, so side effects are often milder and more manageable. Patients on targeted drugs typically report better quality of life and fewer hospital visits.
How do doctors know if a patient is eligible for targeted therapy?
Doctors perform genomic testing on a tumor sample using next-generation sequencing (NGS) panels like FoundationOne CDx or MSK-IMPACT. These tests look for mutations in genes like EGFR, ALK, BRAF, and NTRK. Only patients whose tumors have specific, actionable mutations qualify for targeted drugs. About 13.8% of cancer patients currently meet this criteria.
Why don’t all cancer patients get targeted therapy?
Not all tumors have known targetable mutations. Many cancers lack drugs that can effectively block their drivers. Also, access is limited by cost, insurance coverage, and availability of testing. In the U.S., 65% of advanced cancer patients get genomic testing; in Europe, it’s 22%. Many patients wait weeks for approval or are denied coverage entirely.
Can targeted therapy cure cancer?
In most cases, targeted therapy doesn’t cure cancer - but it can turn it into a chronic condition. For example, patients with chronic myeloid leukemia on imatinib now live nearly normal lifespans. In lung cancer, targeted drugs can extend survival by years. But resistance often develops, requiring new treatments. Long-term control, not cure, is the current goal.
What are the biggest challenges with targeted therapy?
The main challenges are: 1) Only a small percentage of patients have actionable mutations; 2) Tumors often develop resistance within a year; 3) Drugs are extremely expensive; 4) Testing access is unequal across regions and income groups; and 5) We still lack drugs for many common mutations, especially in tumor suppressor genes like TP53.

Been on osimertinib for 18 months. Still walking my dog. Still making coffee without puking. Chemo would’ve put me in a coffin by now. I’m not a miracle - just lucky enough to have the right mutation.
so like... if your DNA is the code and cancer is a glitch... are we just waiting for a software update? 🤔💊 #geneticsisfuture
My aunt got tested after her second round of chemo failed. Found an NTRK fusion. Took larotrectinib. She’s hiking again. No hair loss. No IVs. Just peace. If you’re fighting this - ask for the test. It’s worth it.
Genomic testing should be standard on day one for stage III+ cancers. Not optional. Not a luxury. It’s basic care. Insurance delays cost lives. Stop treating precision medicine like a bonus.
Look, I get it - targeted therapy sounds like sci-fi magic. But let’s be real. You’ve got a 13% chance of even qualifying. Then you wait three weeks for results. Then your insurance says no. Then your tumor mutates again. Then you’re back to chemo. And the drug costs more than my car. This isn’t progress - it’s a high-tech lottery where the house always wins. And don’t even get me started on how they market this as ‘hope’ while billing you $20K a month. I’m not mad. I’m just… tired.
How quaint. We’ve replaced the sledgehammer with a scalpel… but only for the privileged few. The real tragedy isn’t the lack of drugs - it’s the moral bankruptcy of a system that turns life-saving science into a gated community. You don’t get to call this ‘precision medicine’ when your precision only works for those who can afford it. This isn’t innovation - it’s inequality with a lab coat.
My cousin in Indonesia got diagnosed with lung cancer. No testing. No targeted therapy. Just chemo. She passed in six months. Here in the U.S., my friend is alive because her tumor had one tiny glitch in the code. This isn’t science. This is a privilege. And it breaks my heart.
Don’t give up. If you’re reading this and you or someone you love has cancer - ask for the test. Ask again. Ask louder. Find a molecular tumor board. Call patient advocacy groups. There are programs that help with costs. Clinical trials are waiting. You’re not alone. This fight is hard - but you’ve got more power than you think. Keep pushing. You’ve got this.