CBD Drug Interaction Checker
Check Medication Interactions
Enter a medication name to see if it interacts with CBD oil through CYP450 enzyme inhibition.
When you take CBD oil with your prescription meds, something quiet but powerful is happening inside your body-your liver’s enzyme system is being slowed down. This isn’t just a theoretical concern. People are ending up in the hospital because their blood thinners spiked, their seizure meds made them too drowsy, or their painkillers lasted too long. And it’s all tied to one system: the CYP450 enzymes.
What Exactly Is CYP450 and Why Does It Matter?
Your liver has a team of enzymes called cytochrome P450 (CYP450) that break down about 70 to 80% of all prescription drugs. Think of them like molecular scissors. When you take a pill-say, warfarin for blood clots, clobazam for seizures, or sertraline for depression-these enzymes chop it up so your body can get rid of it. Without them, drugs would build up to dangerous levels.
CBD oil doesn’t just float through your system. It steps in and jams those scissors. Research shows CBD strongly inhibits key enzymes like CYP2C9, CYP2C19, and CYP3A4. That means if you’re on a drug processed by one of these, your body can’t clear it fast enough. The result? Higher drug levels in your blood. That’s not always bad-but without monitoring, it’s risky.
Real Cases: When CBD Turns Dangerous
One patient in Ohio started taking 25 mg of CBD oil daily for anxiety. She was already on warfarin to prevent strokes. Within ten days, her INR-a measure of blood clotting-shot from 2.5 to 5.8. Normal is 2-3. Anything above 4.5 puts you at high risk of bleeding. She ended up in the ER needing vitamin K to reverse the effect.
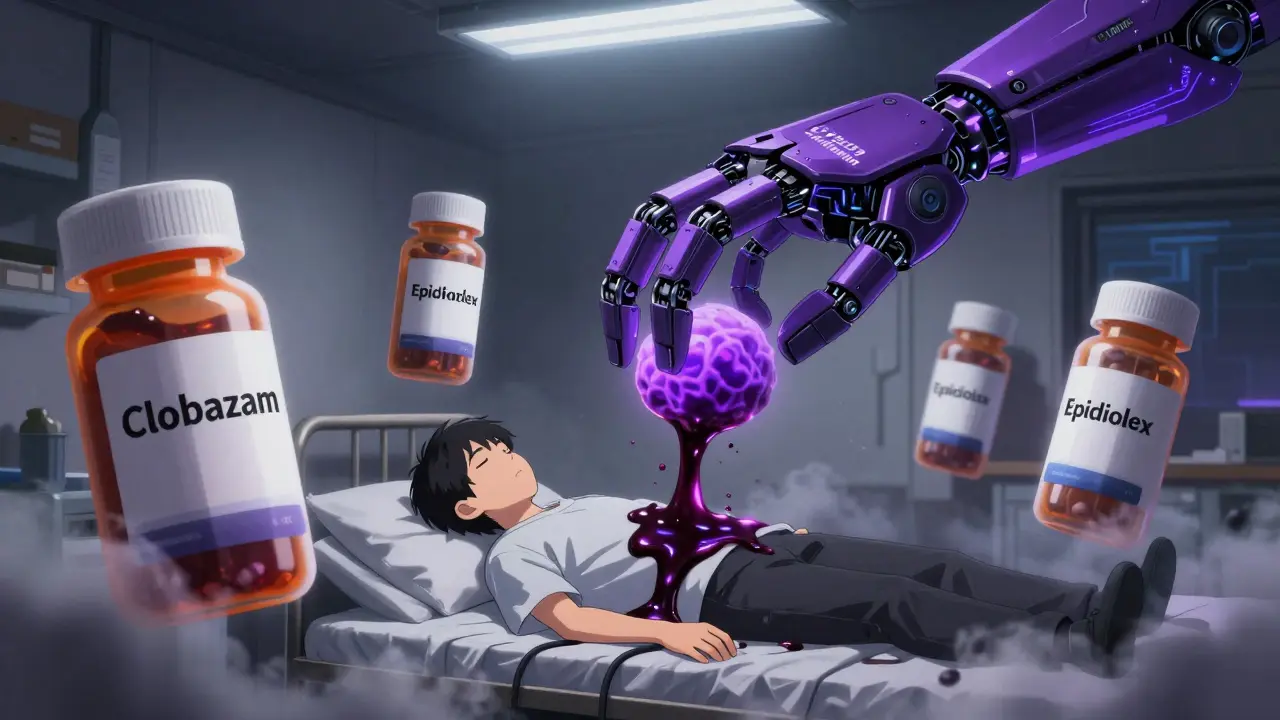
In another case, a teenager with Dravet syndrome began Epidiolex (FDA-approved CBD). His neurologist didn’t adjust his clobazam dose. Within two weeks, his blood levels of the active metabolite jumped 60%. He was sleeping 18 hours a day, barely able to walk. His dose of clobazam had to be cut in half.
These aren’t rare. A 2023 study of 217 medical cannabis users found that 34% experienced increased sedation when mixing CBD with other meds. Among those taking drugs metabolized by CYP2C19-like clobazam, diazepam, or proton pump inhibitors-the rate jumped to 58%.
Which Medications Are Most at Risk?
Not all drugs are affected equally. The big red flags are medications with a narrow therapeutic index-where the difference between a helpful dose and a toxic one is tiny. These include:
- Warfarin (CYP2C9): Risk of dangerous bleeding
- Clobazam (CYP2C19): Extreme drowsiness, confusion
- SSRIs like sertraline and fluoxetine (CYP2D6): Risk of serotonin syndrome
- Statins like simvastatin (CYP3A4): Muscle damage, kidney failure
- Fentanyl and oxycodone (CYP3A4): Respiratory depression
- Calcium channel blockers like amlodipine (CYP3A4): Low blood pressure, dizziness
Even common OTC drugs like ibuprofen (CYP2C9) can become riskier. A 2022 study showed CBD can raise ibuprofen levels by up to 40% in some people.
Why CBD Is Worse Than You Think
Most people assume CBD is safe because it’s "natural." But natural doesn’t mean harmless. CBD is one of the most potent CYP450 inhibitors among cannabinoids. Its IC50 values-the concentration needed to block half the enzyme activity-are in the 0.03-1.0 μM range. Therapeutic doses of CBD (1-2 μM) often hit right in that danger zone.
Even more surprising: it’s not just CBD. Its metabolites-like THC-COO-Gluc, which stays in your blood for days-are also strong inhibitors. So even if you feel "clear-headed," your liver is still being slowed down.
And here’s the kicker: non-prescription CBD products are wildly inconsistent. A 2022 JAMA study found that 42% of products contained less CBD than labeled, while 21% had more. One bottle might have 10 mg per dose. Another, labeled the same, might have 28 mg. You can’t guess what you’re taking.
What About THC, CBG, or Other Cannabinoids?
THC also inhibits CYP450 enzymes, but less broadly than CBD. It hits CYP2C19 hardest-so if you’re on clobazam or diazepam, THC can be just as risky. CBN, often marketed as a sleep aid, strongly blocks CYP2E1 and CYP2B6. CBG and CBDV show some inhibition, but data is limited. CBG appears to be milder, making it a potential alternative for people who need cannabinoids without the drug interaction risk.
But here’s the problem: most products don’t list exact cannabinoid profiles. Even "broad-spectrum" oils may contain unknown amounts of THC or CBN. You’re flying blind.

How to Stay Safe
If you’re on prescription meds and thinking about CBD-or already using it-here’s what to do:
- Talk to your doctor or pharmacist before starting. Don’t assume they know about CBD. Bring the product label.
- Ask if your meds are metabolized by CYP2C9, CYP2C19, or CYP3A4. These are the big three.
- Get a blood test if you’re on warfarin, clobazam, or other narrow-index drugs. Check levels before starting CBD, then again 5-7 days after.
- Start low, go slow. If your doctor approves, begin with 5 mg/day. Wait two weeks. Monitor for drowsiness, dizziness, or unusual side effects.
- Space out doses. Take your medication and CBD at least 3-4 hours apart. This doesn’t eliminate risk, but it can help reduce peak overlap.
- Watch for sedation. If you’re suddenly more tired than usual, or your meds feel stronger, stop CBD and call your provider.
The Bigger Picture
The CBD market hit $28.6 billion in 2023. Over 64 million Americans use it. Yet most products still don’t warn about drug interactions. The FDA has sent warning letters to 15 companies for failing to include these risks on labels. Pharmacists in the U.S. now need 3 hours of continuing education on cannabinoid interactions.
On the positive side, researchers are developing tools to help. The University of Washington is launching a free "Cannabis-Drug Interaction Checker" in mid-2024. Some clinics are already using therapeutic drug monitoring to safely integrate CBD into treatment plans.
And yes-there are cases where CBD helps. One chronic pain patient reduced his fentanyl dose by 40% after CBD slowed its metabolism. But that didn’t happen by accident. It was done under strict medical supervision, with daily blood tests and careful titration.
CBD isn’t the enemy. But treating it like a harmless supplement? That’s the real danger.
What’s Next?
The NIH is running a major study (NCT04893224) testing CBD’s effect on warfarin in 120 volunteers. Results are expected in late 2024. The European Medicines Agency now requires all cannabinoid drugs to include CYP450 interaction data on their labels. In the U.S., that’s still optional for retail products.
Companies like Axim Biotechnologies are testing nanoparticle CBD that avoids liver metabolism entirely. If it works, it could change everything. But for now, if you’re on meds, assume CBD interacts. Don’t gamble with your health.

CBD and warfarin? Bad combo. I saw a guy bleed out from a nosebleed after taking both. Don't be that guy.
So... you're saying natural = dangerous? 😅 That's wild. My grandma takes turmeric and lives to 98. 🌿
Valid points. I’ve been on clobazam for years. Just started 10mg CBD last week. No issues yet, but I’m watching closely.
While the pharmacokinetic data is compelling, it's worth noting that individual metabolic variation significantly modulates risk. Population averages don't always reflect clinical reality.
Oh wow, another ‘CBD is dangerous’ article. Let me guess-written by someone who’s never taken it but reads FDA press releases? People have been using cannabis for millennia. Now we’re scared of a plant compound? 🤦♀️
lol the FDA sent warning letters? Yeah right. My vape pen says 500mg CBD and I’ve been using it for 2 years. Still alive. 😎
I appreciate how thorough this is. My mom is on warfarin and started CBD for arthritis. We got her INR checked right away-went from 2.8 to 3.1. No drama, just monitoring. Knowledge is power.
One must interrogate the epistemological foundations of this discourse: Is ‘safety’ merely a regulatory construct? Or is it an emergent property of biochemical interactivity? The CYP450 system-this molecular cathedral of detoxification-is not merely a ‘scissors’-it is the very locus of metabolic sovereignty. CBD, then, is not an ‘interferer’-it is a silent revolutionary, forcing pharmacology to confront its own arrogance. We medicate with chemical ignorance, then panic when nature reasserts its laws. The real tragedy? We still think a label can contain complexity.
my cousin took cbd with his blood pressure med and passed out. 911 called. he’s fine now. just be careful guys. not worth it.
Let me just say-this is the most terrifying thing I’ve read since I found out my coffee maker was leaking radiation. I’ve been taking 25mg CBD daily for anxiety, plus sertraline, simvastatin, and amlodipine. I thought my brain fog was just ‘adulting.’ Turns out I’m basically running a slow-motion drug overdose. I just stopped the CBD. My hands stopped shaking. My sleep improved. I feel like I’ve been living in a foggy, chemical nightmare and didn’t even know it. I’m not mad-I’m just… stunned. How many people are doing this? How many are dying quietly? This isn’t a ‘warning.’ This is a public health emergency wrapped in a gummy bear.
Hey everyone-this is super important info, and I’m glad someone laid it out so clearly. If you’re on meds and thinking about CBD, talk to your pharmacist. They’re the unsung heroes of drug safety. I work at a pharmacy, and 9 out of 10 people have no idea what their meds do. Bring your bottle. Ask the questions. You’re not being annoying-you’re protecting your life.
i just started cbd for my back pain and im on lexapro and tylenol. i feel a little more tired but i thought it was just stress. maybe i should get my levels checked. thanks for this