Every year, thousands of people end up in the hospital not because of a fall, infection, or heart attack-but because of something they took for a headache, sore knee, or back pain. NSAIDs-like ibuprofen, naproxen, and even low-dose aspirin-are everywhere. You can buy them over the counter. You might take them daily without thinking. But if you’re taking too much, or combining them with other meds, you could be quietly damaging your gut-and bleeding inside without knowing it.
How NSAIDs Hurt Your Stomach (Even When You Feel Fine)
NSAIDs work by blocking enzymes called COX-1 and COX-2. That’s how they reduce pain and swelling. But COX-1 also helps protect the lining of your stomach and intestines. When you take too much, or take it for too long, that protective layer breaks down. It doesn’t always hurt. It doesn’t always make you feel sick. That’s the danger.
Studies show that up to 70% of people who take NSAIDs long-term have visible damage in their gut-erosions, ulcers, tiny bleeding spots-seen during endoscopy. Yet only about 10% of them report any symptoms like heartburn or stomach pain. That means most people don’t know they’re at risk until they start vomiting blood, passing black tar-like stools, or suddenly feel dizzy from internal bleeding.
It’s not just the upper GI tract. NSAIDs can also damage the small and large intestine, leading to bleeding, inflammation, and even malabsorption. The damage is silent, slow, and often ignored until it’s serious.
The Real Risk: Who’s Most Likely to Bleed?
Not everyone who takes NSAIDs will bleed. But some people are at much higher risk. If you fit any of these profiles, you’re in a danger zone:
- You’ve had a stomach ulcer or GI bleed before
- You’re over 65
- You take low-dose aspirin daily for heart protection
- You’re on blood thinners like warfarin, or antiplatelets like clopidogrel
- You take more than one NSAID at a time
- You have an active H. pylori infection
- You take steroids like prednisone along with NSAIDs
The biggest red flag? Combining low-dose aspirin with another NSAID. Research shows this combo triples your risk of a serious GI bleed. Even worse-many people don’t realize aspirin is an NSAID. They think, “I’m just taking aspirin for my heart,” and then grab ibuprofen for their arthritis. That’s a dangerous mix.
One study found that over one-third of patients admitted for GI bleeding were taking over-the-counter aspirin daily-often without telling their doctor. They thought it was safe because it was “low dose.” It’s not.
Why “Low Dose” Aspirin Isn’t Safe Either
Doctors often prescribe 75-100 mg of aspirin daily to prevent heart attacks. That sounds harmless. But here’s the truth: even that small amount increases your risk of GI bleeding by 2 to 4 times. And the higher the dose, the worse it gets. Daily doses of 150 mg raise the risk even more. At 300 mg, the chance of bleeding is nearly four times higher than if you didn’t take it at all.
And here’s something most people don’t know: enteric-coated or buffered aspirin doesn’t help. It doesn’t reduce bleeding risk. The coating might stop it from dissolving in your stomach, but it still damages the gut lining further down. The same goes for “gastroprotective” formulations. They’re marketing, not medicine.
If you’re on daily aspirin, don’t add another NSAID unless your doctor specifically says it’s safe-and even then, you should be on a proton pump inhibitor (PPI) like omeprazole to protect your stomach.

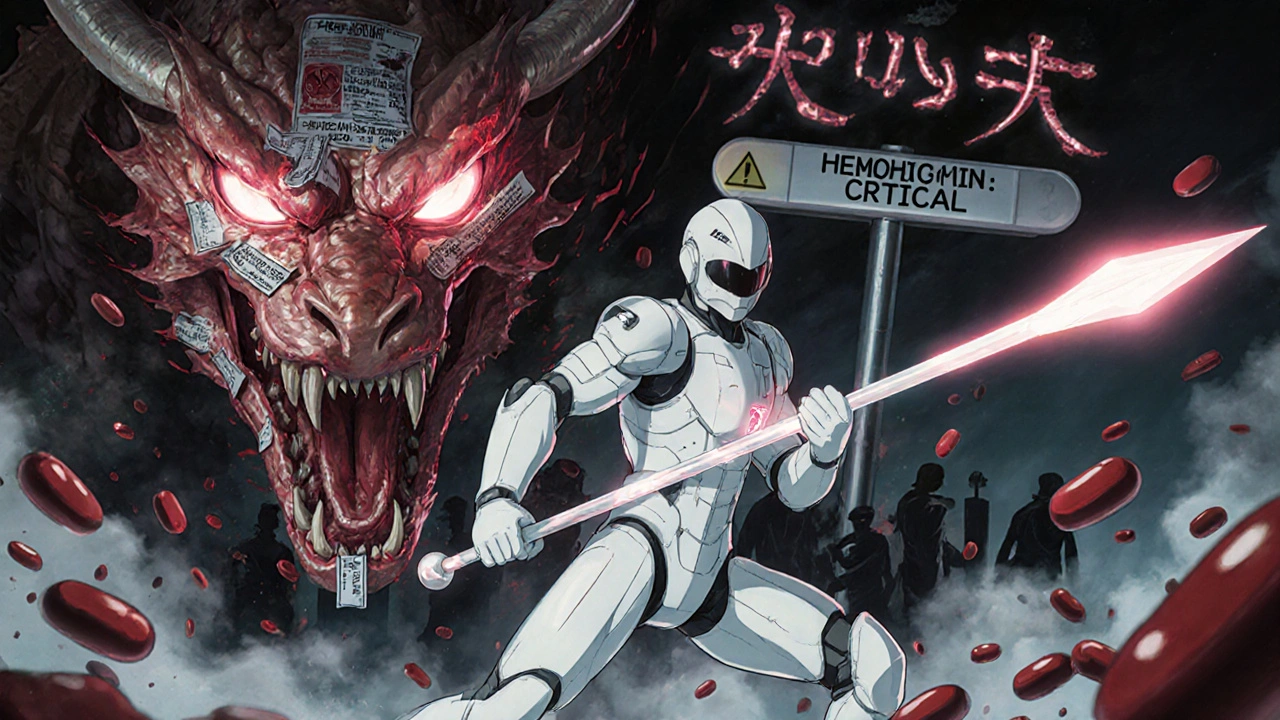
What Happens When You Bleed Inside?
GI bleeding from NSAIDs doesn’t always look like a horror movie. Sometimes it’s obvious: black, tarry stools (called melena), or vomiting bright red blood. But often, it’s hidden. You might feel tired, weak, short of breath. Your lips might look pale. You might get dizzy standing up. That’s not just “getting old”-that’s your body losing blood slowly, day after day.
Doctors call this “occult bleeding.” It doesn’t show up on the outside. But it shows up in your blood tests. Hemoglobin drops. Iron levels crash. You become anemic. And in clinical trials, more than half of NSAID users who became anemic had no visible ulcer or lesion found during endoscopy. That means the bleeding is happening in places hard to see-like the small intestine.
By the time you feel symptoms, you might have lost enough blood to need a transfusion. And if you’re elderly or have heart disease, even a small bleed can trigger a heart attack or stroke.
What Should You Do If You’re Taking NSAIDs?
If you’re on NSAIDs regularly, here’s what you need to do right now:
- Stop taking more than one NSAID at a time. That includes ibuprofen, naproxen, diclofenac, and aspirin. No stacking.
- If you take daily aspirin for heart health, don’t use other NSAIDs unless your doctor approves it. And if they do, you should be on a PPI.
- Ask your doctor if you need a PPI. Proton pump inhibitors like omeprazole or pantoprazole can cut your risk of stomach ulcers by up to 80%-but only if you’re high-risk. They don’t protect your small intestine, but they help with the upper GI tract.
- Get tested for H. pylori. If you have it, treating it reduces your bleeding risk significantly.
- Don’t ignore fatigue, pale skin, or unexplained dizziness. Get a blood test for hemoglobin and iron.
- Keep a list of all your meds-prescription, OTC, supplements-and review it with your doctor every 6 months.
And if you’re thinking, “I only take it once in a while,” that’s still risky. A single high dose of NSAIDs can trigger bleeding in people with hidden ulcers. There’s no safe “occasional” use if you’re in a high-risk group.
What Are the Alternatives?
You don’t have to live with pain. There are safer options:
- Acetaminophen (paracetamol) for pain relief-no GI risk, but watch your liver dose.
- Topical NSAIDs like gels or patches-they deliver the drug to the joint without flooding your gut.
- Physical therapy, heat/cold therapy, or acupuncture for chronic pain.
- For arthritis: disease-modifying drugs or corticosteroid injections, under medical supervision.
If you have chronic pain, talk to your doctor about a pain management plan that doesn’t rely on daily NSAIDs. There are better ways.
When to Go to the Emergency Room
If you’re taking NSAIDs and experience any of these, go to the ER immediately:
- Black, tarry, or bloody stools
- Vomiting blood or material that looks like coffee grounds
- Sudden dizziness, fainting, or rapid heartbeat
- Severe abdominal pain or swelling
- Unexplained fatigue, pale skin, or shortness of breath
Don’t wait. Don’t assume it’s “just indigestion.” Internal bleeding from NSAIDs can kill you in hours if left untreated.
Bottom Line: NSAIDs Are Not Safe by Default
NSAIDs are not harmless. They’re powerful drugs with serious side effects. Millions of people take them without knowing the risks. The medical community has known for decades that these drugs cause GI bleeding-and that most of those cases are preventable.
If you’re on NSAIDs daily, especially with aspirin, steroids, or blood thinners-you’re playing with fire. The damage builds silently. The symptoms hide. The bleeding doesn’t wait for a warning.
Check your meds. Talk to your doctor. Get tested. Don’t assume because it’s over the counter, it’s safe. Your gut doesn’t care how you bought it. It only cares how much you took-and how long you kept taking it.

I never realized how sneaky NSAIDs can be. I take ibuprofen for my back pain and thought it was harmless since it’s OTC. Now I’m checking my meds list with my doctor tomorrow. Thanks for laying this out so clearly - this is the kind of info people need to hear before it’s too late.
Also, I had no idea enteric-coated aspirin doesn’t help. That’s wild. Marketing tricks are everywhere.
Anyone else feel like we’re just told to ‘take it easy’ with pain meds while the real risks are buried in fine print?
Big Pharma knows this. They don’t care. They profit from your bleeding stomach.
It’s frankly irresponsible that these drugs are sold over the counter like candy. People don’t read the warnings. They don’t understand physiology. They just want the pain to go away. And now hospitals are filled with people who thought ‘low dose’ meant ‘safe.’ This isn’t a medical issue - it’s a cultural failure of basic responsibility.
Y’all are acting like NSAIDs are some kind of poison bomb. Chill the hell out. I’ve been taking naproxen for 15 years. My stomach’s fine. My knees are functional. You think the world’s gonna end because someone pops an Advil? Get a grip. This is fearmongering dressed up as ‘public health.’
And yeah, aspirin’s an NSAID - so what? Millions of people take it. Most of us don’t turn into walking blood bags. Stop scaring people into thinking every pill is a death sentence.
Why is the government letting this happen I mean really who’s in charge here I take ibuprofen every day for my back and now I’m scared to death because some guy on the internet says I’m gonna bleed out I dont even know what a PPI is but I guess I need one now I just want to walk without pain damn it
I live in India and here people use painkillers like water. My uncle takes diclofenac daily for his arthritis and never saw a doctor. He got anemic last year and didn’t know why. Now he’s on iron and omeprazole. I showed him this post and he finally listened. We need more of this awareness in places where doctors are far away and pills are cheap.
Also paracetamol is better for us here. Less side effects. And cheaper too.
Let’s be brutally honest: this isn’t about ‘awareness.’ It’s about liability. Hospitals and drug companies know the risks. They’ve known for decades. But they don’t want to scare people away from sales. So they bury the facts in 50-page PDFs nobody reads. And then they blame the patient for ‘not reading the label.’
Meanwhile, the FDA approves new NSAID formulations every year - all while quietly ignoring the 200+ peer-reviewed studies linking them to silent GI damage. This is systemic negligence. And you’re all just… accepting it.
This post made me cry a little. I had a cousin who bled out from an NSAID overdose and no one knew until it was too late. She was 42. Took aspirin for headaches and ibuprofen for cramps. Thought she was being smart by alternating them. 😔
Thank you for writing this. I’m sharing it with my whole family. And I’m finally asking my doctor about a PPI - I’m over 60 and on low-dose aspirin. I didn’t realize I was in the danger zone.
Also, topical NSAIDs are a game changer. I use the gel for my knee now - no stomach drama. 🙏