Lithium Toxicity Risk Calculator
Current Lithium Level
Risk Assessment
Estimated Lithium Level: 0.00 mmol/L
For safe lithium management, you should:
- Monitor your lithium levels every 3-6 months if stable
- Never start new medications without consulting your doctor
- Watch for early symptoms: tremors, nausea, dizziness, confusion
Take lithium for bipolar disorder? You’re not alone. Around 750,000 Americans rely on it every day. But here’s the catch: a simple over-the-counter painkiller or a common blood pressure pill can push your lithium levels into the danger zone-fast. And you might not even feel it until it’s too late.
Why Lithium Is So Dangerous
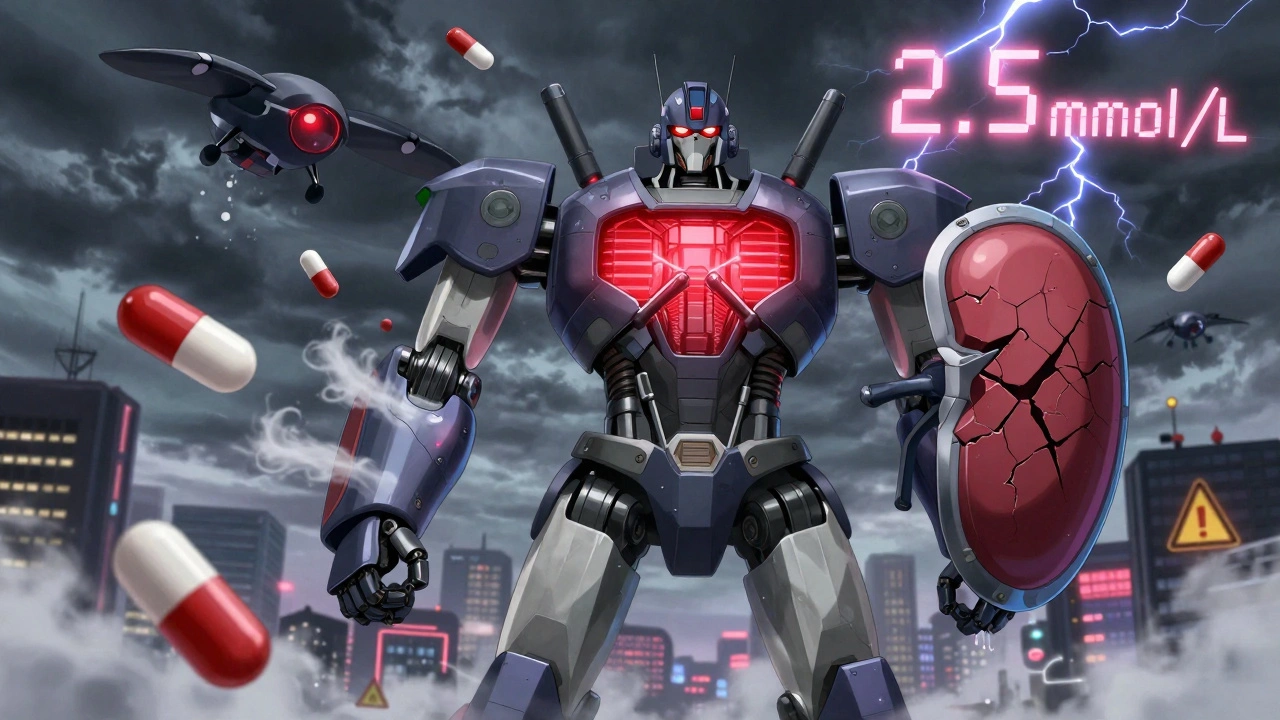
Lithium isn’t like other meds. It doesn’t get broken down by your liver. Instead, your kidneys filter it out, almost entirely unchanged. That sounds simple, but it’s actually a huge risk. Your kidneys have to get the balance just right. Too little lithium? Your mood can crash. Too much? You could end up in the hospital-or worse. The safe range? Between 0.6 and 1.2 mmol/L. Cross 1.5 mmol/L, and you’re in mild toxicity. At 2.0 mmol/L, symptoms get serious: tremors, confusion, nausea. Hit 2.5 mmol/L or higher? That’s a medical emergency. You might need dialysis. Some patients have died from this. And here’s the scary part: you don’t need to take a huge overdose. Just a small change in how your kidneys handle lithium-often caused by another medication-and your levels can spike overnight.Diuretics: The Silent Lithium Killer
Diuretics, or water pills, are among the most dangerous partners for lithium. They’re often prescribed for high blood pressure, heart failure, or swelling. But they interfere with your kidneys’ ability to clear lithium. Thiazide diuretics like hydrochlorothiazide and bendroflumethiazide are the worst offenders. They cause lithium levels to jump by 25% to 40%, sometimes even fourfold. That’s not a typo. One study found 75-85% of patients on thiazides saw dangerous lithium increases. And it happens fast-within 3 to 5 days. Why? Thiazides act on the part of the kidney where lithium gets reabsorbed. Normally, your body reabsorbs only a small amount of lithium. Thiazides trick your kidneys into holding onto even more. The result? Lithium builds up like water in a clogged sink. Loop diuretics like furosemide are a little safer, but still risky. They raise lithium levels by 10-25%, especially if you already have kidney trouble (eGFR below 60). So if you’re on furosemide and lithium, your doctor should be checking your levels every 4-5 days at first.NSAIDs: The Over-the-Counter Trap
NSAIDs-like ibuprofen, naproxen, and indomethacin-are everywhere. You grab them for headaches, back pain, or menstrual cramps. But if you’re on lithium, they’re a ticking time bomb. These drugs block prostaglandins, which help keep your kidneys filtering properly. Less prostaglandin? Lower blood flow to the kidneys. That means less lithium gets cleared. Levels rise by 15-30% with ibuprofen. With indomethacin? Up to 40%. That’s enough to push someone from safe to toxic in just a few days. Here’s the kicker: many people don’t realize they’re taking NSAIDs. Advil, Motrin, Aleve-they’re all NSAIDs. And if you’re self-medicating for pain, your psychiatrist might never know. A 2017 case in New Zealand showed a 72-year-old woman taking lithium and ibuprofen. Her lithium level jumped from 0.8 mmol/L to 1.9 mmol/L in seven days. She died. Autopsy confirmed lithium toxicity. She hadn’t had a blood test in months. Celecoxib is the exception. It’s a COX-2 inhibitor and causes only a 5-10% rise in lithium levels. If you absolutely need an NSAID, this one is the least risky. But even then, your doctor should monitor you closely.
Other Medications That Can Worsen Lithium Toxicity
It’s not just diuretics and NSAIDs. Other common drugs also interfere:- ACE inhibitors (like lisinopril) and ARBs (like valsartan): These blood pressure drugs raise lithium levels by 10-25%. They reduce kidney filtration, just like NSAIDs.
- Calcium channel blockers (like verapamil): They don’t raise lithium levels much, but they can make side effects like tremors and ringing in the ears much worse.
- Antidepressants (especially SSRIs like fluoxetine): Some increase lithium levels, others worsen side effects. Always check before starting one.
- Herbal supplements: The NHS warns there’s no safety data for most herbs with lithium. Ginger, turmeric, ginkgo-none are proven safe.
What Should You Do? A Clear Action Plan
If you’re on lithium, here’s what you need to do right now:- Never start a new medication-even an OTC one-without telling your doctor. That includes painkillers, cold meds, or supplements.
- Get your lithium levels checked every 3-6 months if you’re stable. But if you start a diuretic, NSAID, or blood pressure drug, check every 4-5 days for the first week, then weekly for the first month.
- Know your numbers. Ask your doctor what your personal target range is. Some people need to stay closer to 0.6, others can handle 1.0. Don’t assume everyone’s the same.
- Watch for early signs. Tremors, nausea, frequent urination, dizziness, or confusion? Call your doctor immediately. Don’t wait for a blood test.
- If you need a diuretic, ask if furosemide is an option instead of hydrochlorothiazide. It’s less risky.
- If you need pain relief, avoid ibuprofen and naproxen. Try acetaminophen (paracetamol) instead. If you must use an NSAID, pick celecoxib-and only with close monitoring.

What Happens If Toxicity Strikes?
If your lithium level hits 2.5 mmol/L or higher and you’re confused, vomiting, or having seizures, you need emergency care. Standard treatment includes:- Stopping lithium immediately
- IV fluids to flush it out
- Electrolyte correction
- Hemodialysis if levels are very high or symptoms are severe
The Future: Better Monitoring, Safer Lithium
There’s hope. In 2023, the FDA approved a new home-monitoring device called LithoLink™. It lets you test your lithium levels with a finger-prick and send results directly to your doctor. No more waiting for clinic appointments. Researchers are also testing nano-encapsulated lithium citrate. Early trials show it’s 40% less affected by NSAIDs like ibuprofen. That could be a game-changer. Meanwhile, genetic studies are uncovering why some people are more sensitive. If you’re a poor metabolizer of CYP2D6, you might need even lower doses when taking NSAIDs. Personalized medicine is coming-and fast.Bottom Line: Lithium Works. But It Demands Respect
Lithium is still the most effective mood stabilizer for preventing suicide in bipolar disorder. Studies show it cuts suicide risk by 44% compared to placebo. That’s powerful. But it’s not a drug you can take and forget. It needs constant attention. Your kidneys are your lithium’s only exit route. Anything that slows them down-diuretics, NSAIDs, even dehydration-can turn your treatment into a life-threatening situation. Talk to your doctor. Get tested. Know your meds. Don’t let a painkiller or a water pill undo everything you’ve worked for.Can I take ibuprofen if I’m on lithium?
It’s not recommended. Ibuprofen can raise lithium levels by 15-30%, which can push you into toxicity. If you need pain relief, use acetaminophen (paracetamol) instead. If you absolutely must take ibuprofen, your doctor should check your lithium levels every 4-5 days for the first week and reduce your lithium dose by 15-20%.
What diuretic is safest with lithium?
Furosemide (a loop diuretic) is safer than thiazides like hydrochlorothiazide. Thiazides increase lithium levels in 75-85% of patients, while furosemide raises them in only 15-25%. Still, furosemide isn’t risk-free. Lithium levels must be monitored closely, especially if you have kidney issues.
How often should lithium levels be checked?
If you’re stable and not taking interacting drugs, check every 3-6 months. But if you start a diuretic, NSAID, ACE inhibitor, or any new medication, check every 4-5 days for the first week, then weekly for the first month. Always check after any dose change.
Can lithium toxicity happen without symptoms?
Yes. Many people don’t feel anything until their lithium level is dangerously high. That’s why regular blood tests are non-negotiable. A level of 1.8 mmol/L might not cause symptoms, but it’s still toxic. Never rely on how you feel-always rely on lab results.
Are herbal supplements safe with lithium?
No one knows for sure. The NHS and other health agencies warn that there’s no reliable safety data for herbal remedies with lithium. Supplements like St. John’s wort, ginkgo, or turmeric could interfere with lithium levels or worsen side effects. Always tell your doctor what you’re taking-even if it’s labeled "natural."
What should I do if I miss a lithium dose?
If you miss one dose, take it as soon as you remember-unless it’s close to your next dose. Don’t double up. Missing doses won’t cause toxicity, but it can make your mood unstable. If you miss multiple doses or are sick with vomiting or diarrhea, contact your doctor. Your body’s lithium clearance changes when you’re dehydrated, which can trigger toxicity even if you haven’t taken extra pills.
Been on lithium for 12 years. Never realized how many everyday meds can mess with it. Learned the hard way after taking Advil for a headache and ending up in ER. Now I keep a list of safe alternatives on my phone. Seriously, if you’re on this med, treat it like a live wire.
Don’t guess. Ask.
Let me be very clear: if you're taking lithium, you are not allowed to take NSAIDs without explicit medical supervision. Period. The risk isn't theoretical-it's documented, predictable, and deadly. I've seen patients with stable levels for years crash into toxicity after one weekend of ibuprofen for back pain. It's not a coincidence. It's pharmacokinetics. Your kidneys are not 'adjusting'-they're being hijacked. Check your levels before, during, and after any new med. And if your doctor doesn't know this? Find a new one.
My mom’s on lithium and just started furosemide for heart failure. Her doctor didn’t mention the interaction until I brought it up. She’s lucky. So many people get prescribed these combos without a second thought. I printed out the FDA warning and gave it to her prescriber. They adjusted her dose and started weekly labs. If you’re a caregiver or patient-speak up. No one else is watching.
I’ve been on lithium since I was 19. I’m 37 now. I’ve had two near-misses-one with a cold med that had pseudoephedrine, another with a friend’s ‘natural’ joint supplement. I keep a medication log in my Notes app. I screenshot every new script and send it to my psych team. I don’t care if it seems obsessive. I’d rather be annoying than dead. If you’re on lithium, you’re not just managing a mood disorder-you’re managing a minefield. Treat it like it.
It’s frankly irresponsible that these drugs are sold over the counter without warnings. I mean, really? Ibuprofen? A drug that can kill someone on lithium? And people just pop them like candy. This isn’t a medical issue-it’s a societal failure. Where’s the public health campaign? Where’s the mandatory labeling? The FDA should be ashamed. And yet, here we are, patients left to educate ourselves while Big Pharma profits from the ignorance they’ve cultivated. I’m not mad. I’m just… profoundly disappointed in humanity.
Thank you for this detailed and life-saving post. As someone who works in primary care, I see this mistake happen too often. Patients think 'natural' means safe. They think 'over-the-counter' means harmless. They think 'I've taken this before' means it's fine. We need better systems. I now have a checklist in my EMR that flags lithium patients when NSAIDs, diuretics, or ACE inhibitors are prescribed. It’s a small thing-but it saves lives. Please, if you're on lithium, don't rely on memory. Write it down. Tell your pharmacist. Print this article. Share it.
My brother took hydrochlorothiazide for high blood pressure while on lithium. He didn’t feel different. No tremors. No nausea. Just a little tired. His blood test came back at 2.1. He was in the hospital for five days. Now he’s on losartan instead. He’s fine. But he almost didn’t make it. This isn’t a 'maybe' thing. It’s a 'when' thing. If you’re on lithium and your doctor prescribes a diuretic, ask: 'Is this the safest option?' If they say 'probably,' walk out. Find someone who knows the stakes.
I used to think lithium was just a 'mood stabilizer' until I saw my best friend spiral into confusion, vomit blood, and get dialyzed. She didn’t know she was on a dangerous combo. No one told her. She thought her headaches were just stress. I’ve been pushing this info on every bipolar person I know. If you’re reading this and you’re on lithium-do not ignore this. Save your life. Don’t wait for a crisis. Get tested. Talk to your pharmacist. Print this. Hang it on your fridge.
Just got my new LithoLink™ device. It’s like a glucose meter but for lithium. I prick my finger, wait 90 seconds, and my doctor gets the result instantly. No more waiting two weeks for a lab. No more guessing. I feel like I have control again. I’ve been on lithium for 18 years and this is the first time I’ve felt truly safe. If your doctor doesn’t know about this device-tell them. It’s FDA-approved. It’s real. It’s here. Don’t settle for outdated monitoring.
I’ve been on lithium for 20 years. I’ve had three hospitalizations. I’ve lost friends to this. I’ve watched people die because they took Aleve for a sprained ankle. I’m not exaggerating. I’m not dramatic. I’m just tired. Tired of seeing people treat this like a casual medication. Tired of doctors who don’t know the risks. Tired of patients who think 'I feel fine' means 'I’m safe.' I don’t want to be the guy who tells you how to live. I just want you to live. Please. Get tested. Don’t take ibuprofen. Don’t trust 'natural.' Don’t wait for symptoms. Lithium doesn’t warn you. It just kills you.
So let me get this straight-you’re telling me that a drug that's been around since the 1940s is still being prescribed without mandatory warning labels? And the FDA just approved a home test kit now? What took them so long? And why is this only coming out now? I’m starting to think this whole thing is a cover-up. Big Pharma doesn’t want you to know how dangerous this is. They profit from your suffering. They profit from your dialysis. They profit from your funeral. This isn’t medicine. It’s a controlled demolition. And they’re letting us walk into the building.
While the clinical data presented is accurate, the framing of this post is dangerously reductionist. Lithium toxicity is not merely a pharmacokinetic issue-it is a metaphysical one. The body, in its intricate design, is not a machine to be calibrated with blood tests. The true danger lies not in NSAIDs or diuretics, but in the modern medical paradigm’s obsession with quantification over qualitative lived experience. When we reduce a human being to a serum concentration, we abandon the soul’s wisdom. Perhaps the real toxicity is not in the lithium-but in the system that demands we measure it.
Just want to add: if you're on lithium and need pain relief, acetaminophen is your best bet-but even that’s not zero-risk. Recent studies show that chronic high-dose APAP can cause mild renal impairment, which might indirectly affect lithium clearance. So don’t go overboard. 325mg every 6 hours max. And if you’re on a beta-blocker for tremors, remember: it masks symptoms. You might feel fine while your lithium level climbs. Always check labs. Don’t trust your nerves. Trust the numbers.