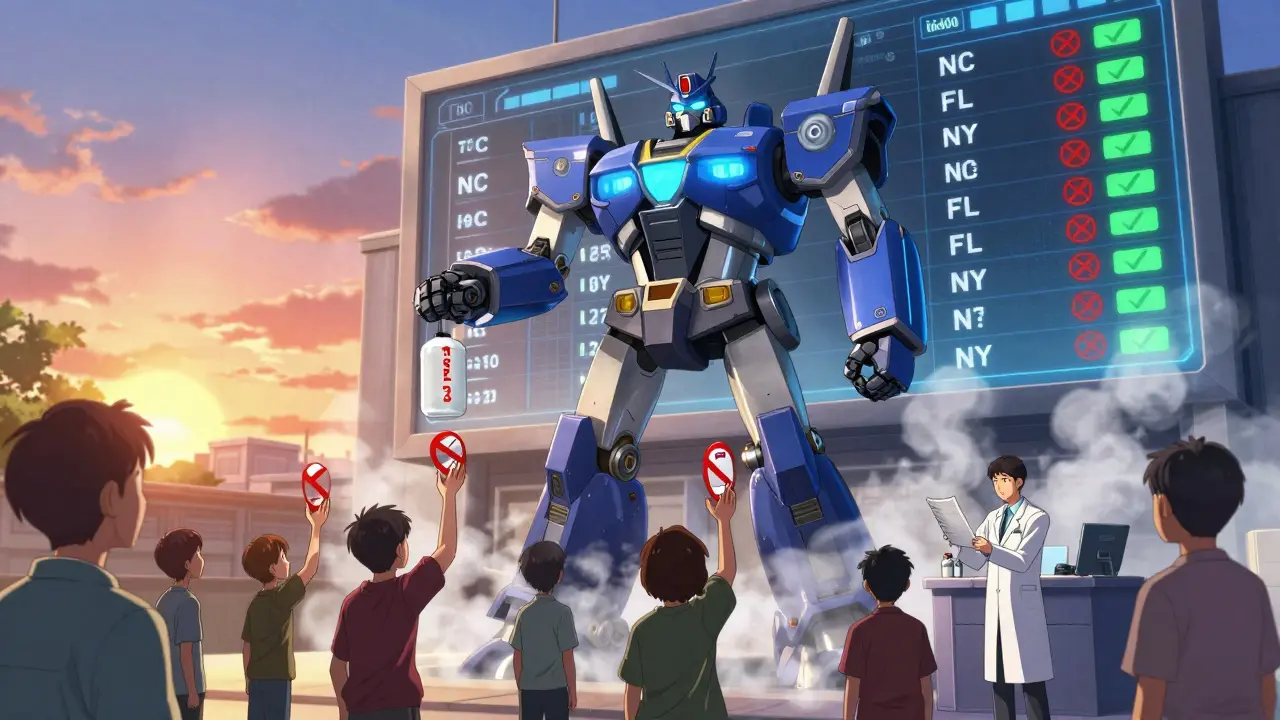
When you’re on Medicaid, getting your prescriptions shouldn’t mean choosing between medicine and groceries. But understanding what’s covered-and what’s not-can feel like navigating a maze. In 2026, Medicaid still covers prescription drugs for nearly 85 million low-income Americans, but the rules vary wildly from state to state. What’s covered in North Carolina isn’t always covered in Florida. And even within the same state, the drug you need might require jumping through hoops before you can get it.
Medicaid Covers Prescriptions-But Not Always the Way You Expect
Federal law doesn’t require states to cover outpatient prescription drugs under Medicaid. Yet every single state does. Why? Because without drug coverage, people skip doses, end up in the ER, and cost the system more in the long run. The real story isn’t whether drugs are covered-it’s how they’re covered. Most states use a Preferred Drug List (PDL), which sorts medications into tiers. Tier 1 usually means generic drugs with the lowest copay-often $1 to $5. Tier 2 is brand-name drugs that cost more, maybe $15 to $40. Tier 3? That’s for specialty drugs, like those for rheumatoid arthritis or hepatitis C. Those can cost $100 or more, even with Medicaid. Here’s the catch: just because a drug is on the list doesn’t mean you can walk in and get it. Many states require step therapy-you have to try and fail on two cheaper, preferred drugs before they’ll cover the one your doctor originally prescribed. If your doctor wants to prescribe Wellbutrin XL for depression, but you haven’t tried two other SSRIs first? You’ll get denied. Unless you have a rare condition, or your doctor files a prior authorization with clinical notes proving why the cheaper options won’t work.What’s Not Covered? The List Changes Often
Medicaid formularies aren’t static. They change every few months. In North Carolina, for example, drugs like Vasotec, Trulance, and Uceris were removed from the preferred list in 2025 because the state couldn’t get a good enough rebate from the manufacturer. That doesn’t mean they’re banned-but now you need prior authorization just to get them, and even then, approval isn’t guaranteed. Some drugs get moved from preferred to non-preferred status. Epidiolex®, a medication for rare epilepsy syndromes, was moved out of Tier 1 in July 2025. That meant a beneficiary’s monthly copay jumped from $5 to $45. No warning. No notice. Just a formulary update posted online. And then there are drugs that are simply excluded. Over-the-counter painkillers? Not covered. Cosmetics? Nope. Weight-loss drugs like Ozempic? Only if prescribed for diabetes-not for weight loss alone. Even then, prior authorization is almost always required.Prior Authorization: The Hidden Barrier
Prior authorization is the most common reason people delay or skip their meds. It’s when your doctor has to call or submit paperwork to prove your drug is medically necessary. In 2024, the Medicare Rights Center found that 63% of Medicaid beneficiaries waited longer than a week to get approval for a non-preferred drug. Some waited over two weeks. The process is exhausting. Your doctor has to fill out forms, attach lab results, sometimes even write a letter explaining why you can’t use the preferred alternative. If the paperwork is incomplete? Denied. You start over. If you’re on disability, working two jobs, or caring for kids? You don’t have time for this. But here’s the good news: 78% of denials are overturned on appeal-if you submit complete clinical documentation. That means your doctor’s notes need to be specific: not just “patient needs this drug,” but “patient tried Drug A and B, experienced nausea and dizziness, labs show no improvement in HbA1c.” Generic statements won’t cut it.
Costs Are Lower Than You Think-If You Know How to Access Them
Medicaid doesn’t just cover your drugs-it often pays for them at a discount. Thanks to the Medicaid Drug Rebate Program, drugmakers pay the government a cut of every pill sold. That’s how states keep costs down. In 2025, generics made up 89% of all Medicaid prescriptions but only 27% of the total spending. That’s because the rebate system pushes prices way below retail. If you qualify for Extra Help (a federal program for low-income Medicare beneficiaries who also have Medicaid), your out-of-pocket costs drop even further. In 2026, you pay $0 for generic drugs up to $4.90 per prescription and $12.15 for brand names-until you hit $2,000 in annual spending. After that? You pay nothing. And you can change your drug plan once a month, not just once a year. But here’s the problem: 1.2 million eligible people don’t even know they qualify. If you’re on Medicaid, you’re automatically eligible for Extra Help. You don’t need to apply. Yet many don’t get it because no one told them.State-by-State Differences Matter More Than You Realize
North Carolina requires you to fail two preferred drugs before moving to a non-preferred one. Florida? They have a separate list for drugs administered by doctors-like injections for MS or cancer. New York lets you skip step therapy for mental health meds if your doctor says it’s unsafe. Texas has tighter limits on opioid prescriptions. There’s no national standard. Each state negotiates its own deals with pharmacy benefit managers (PBMs) like CVS Caremark, Express Scripts, and OptumRx. That’s why a drug covered in Ohio might be denied in Georgia. It’s not about medical need-it’s about what rebate the state got. If you move states, your coverage can change overnight. That’s why it’s critical to check your state’s current formulary every time you get a new prescription. You can find it on your state’s Medicaid website or through your PBM’s portal.
How to Get Your Prescription Without the Headache
Here’s how to avoid delays and denials:- Always use a network pharmacy. Mail-order is often cheaper for maintenance meds.
- Ask your doctor to check the formulary before prescribing. Many have access to real-time formulary tools.
- If denied, appeal immediately. Keep copies of everything.
- Call your state’s SHIP (State Health Insurance Assistance Program) hotline. They help for free.
- Ask if you qualify for Extra Help-even if you’re on Medicaid, you might not know it.
What’s Coming in 2026?
The federal government is pushing for change. In early 2026, CMS will require states to prove their formularies don’t block medically necessary drugs. That could mean fewer step therapy rules and more transparency. The Inflation Reduction Act’s $2,000 out-of-pocket cap for Medicare Part D also affects dual-eligible patients (those on both Medicare and Medicaid). If you’re one of them, you’ll benefit from lower costs even if your Medicaid plan doesn’t fully cover your drug. But the big threat? New gene therapies. Twelve to fifteen are coming between 2025 and 2027, each costing over $2 million per treatment. States are scrambling. Some are signing outcomes-based contracts-paying only if the drug works. Others are limiting access until they can prove affordability.Bottom Line
Medicaid does cover prescription drugs-but coverage isn’t the same as access. The system works if you know the rules. Use your doctor. Ask questions. Appeal denials. Check your state’s formulary every six months. And if you’re confused, call your state’s SHIP hotline. You’re not alone. Millions of people are navigating the same maze. And with the right info, you can get your meds without the stress.Does Medicaid cover all prescription drugs?
No. Medicaid covers most prescription drugs, but each state has its own formulary-called a Preferred Drug List-that determines which drugs are covered and under what conditions. Some drugs are excluded entirely, and others require prior authorization or step therapy before approval.
Why was my prescription denied by Medicaid?
Common reasons include: the drug isn’t on your state’s formulary, you haven’t tried cheaper alternatives first (step therapy), or your doctor didn’t submit enough clinical documentation. Denials can often be overturned with a proper appeal and detailed medical records from your provider.
How do I find out what drugs Medicaid covers in my state?
Visit your state’s Medicaid website and search for “Preferred Drug List” or “Formulary.” You can also call your state’s State Health Insurance Assistance Program (SHIP) or ask your pharmacy to check your plan’s formulary before filling your prescription.
Can I get my medication cheaper through Extra Help?
Yes-if you qualify. If you have full Medicaid coverage, you’re automatically eligible for Extra Help, which caps your monthly copays at $4.90 for generics and $12.15 for brand-name drugs. After spending $2,000 in a year, you pay $0 for covered drugs. Many people don’t realize they qualify, so check with your state Medicaid office.
Do I have to use a specific pharmacy to get my Medicaid-covered drugs?
Yes. You must use a pharmacy that’s in your Medicaid plan’s network. Many plans encourage or require mail-order for maintenance medications like blood pressure or diabetes drugs, as it’s often cheaper and more convenient. Ask your plan or pharmacist for a list of in-network pharmacies.
How often do Medicaid formularies change?
Formularies are updated at least twice a year-often in January and July-and sometimes more frequently. Some states make off-cycle changes if a drug’s rebate drops or a new generic becomes available. Always check your formulary before starting a new medication.
Are specialty drugs covered under Medicaid?
Yes, but coverage is stricter. Specialty drugs-for conditions like MS, cancer, or rare diseases-are often placed in Tier 3 or higher and require prior authorization, step therapy, and sometimes proof of failure on other treatments. Even then, not all specialty drugs are covered, and some states limit the quantity or duration of use.
What should I do if I can’t afford my Medicaid-covered drug?
First, ask your doctor if there’s a preferred alternative on your state’s formulary. If not, request a prior authorization appeal with clinical documentation. You can also contact your state’s SHIP program for free counseling, or ask your pharmacy about patient assistance programs from drug manufacturers.
Okay but can we just talk about how insane it is that we’re making people jump through hoops just to get their depression meds? 😭 I had a friend who waited 3 weeks for Wellbutrin because she had to try 4 other SSRIs first-she almost relapsed. And then when she finally got it? Her copay jumped from $5 to $45 because the formulary changed without a single email or notice. This isn’t healthcare-it’s a game of Russian roulette with your mental health. 🤯
Stop crying about $5 copays. You think your $12.15 brand-name drug is expensive? Try living in a country where you pay $500 for the same pill. Medicaid is a welfare program-not a luxury concierge service. If you can’t afford meds, don’t have kids, get a job, or move to a state that doesn’t waste money on people who won’t lift a finger. 🤷♂️
Wow, this is so interesting, but... I am from India, and here, we don't have Medicaid, but we have Ayushman Bharat, which covers some drugs, but not all, and sometimes the drugs are out of stock, or the pharmacy says 'this is not in list' even if it is... so I feel you, but also, maybe this is universal? 😅 I mean, why is it so hard everywhere? Also, I think 'prior authorization' should be called 'prior frustration' lol
It’s not about the drugs. It’s about control. The system doesn’t want you to be healthy-it wants you to be dependent. They profit from your suffering. The rebates? The PBMs? The tiers? It’s all a distraction. You’re not fighting for medicine-you’re fighting a machine that was never designed to heal you. 💔
my doctor just told me to check my states formulary and i was like... wait what? i thought medicaid just covered stuff? turns out nope. now i gotta google like a detective just to get my blood pressure pill. why is this so complicated??
The structural inefficiencies inherent in state-level formulary management are a direct consequence of decentralized fiscal autonomy coupled with opaque PBM negotiations. The absence of a unified national pharmacoeconomic framework creates cascading access disparities. Step therapy protocols, while cost-containment mechanisms, function as de facto rationing tools that disproportionately impact vulnerable populations with complex comorbidities. The rebate model incentivizes formulary inclusion based on financial leverage, not clinical utility. This is not a healthcare system-it’s a market-driven allocation engine with catastrophic equity failures.
the fact that you have to appeal a denial just to get your meds is insane. and yet... no one talks about it. i mean, imagine if you had to file paperwork to get a bandaid. 🤦♂️ also, i think the system is designed to make you give up. and most people do. and then they end up in the er. and then the system spends 10x more. genius.
They’re hiding something. The rebates, the PBMs, the sudden formulary changes-it’s all connected. I read that one PBM executive made $80 million last year. Meanwhile, my cousin had to skip her insulin for three weeks because the state switched to a cheaper generic that made her sick. Coincidence? I think not. This isn’t about cost-it’s about power. And they’re laughing all the way to the bank.
bro i used to work at a pharmacy and let me tell u-most docs don’t even know the formulary. they just write scrips like its 2005. i had a lady come in for her RA med and i told her ‘yo this got yanked last week’ and she looked at me like i spoke alien. then i showed her the link and she cried. we need a damn app that auto-checks before the doc hits send. also, Extra Help? yeah its free but no one tells you. its like a hidden cheat code for life.
the step therapy thing is wild. my therapist told me to try 3 other antidepressants before letting me have the one that actually works. i was like ‘but i tried those in 2020 and they made me feel like a zombie’ and she said ‘well, we gotta follow protocol.’ so i waited 6 weeks. lost my job. got evicted. then they approved it. but now i’m on disability. so... congrats system? you win.
so if i’m on medicaid and have extra help... does that mean i can get ozempic for weight loss if i have diabetes? or is that still a no? i’ve been reading conflicting stuff. also, can you change your plan monthly? like, if i find a better one next week, can i just switch? or is that a myth?
Okay, so let me get this straight-you’re telling me that in North Carolina, you have to fail two drugs before getting the one your doctor prescribed, but in New York, you can skip that for mental health meds? And yet, both states are funded by the same federal government? That’s not ‘state flexibility’-that’s a broken, chaotic, arbitrary system that treats people like lab rats. And now you want to add $2 million gene therapies into the mix? What happens when the state says ‘we can’t afford to cure you’? Are we just supposed to die quietly? 😒