Digoxin-Amiodarone Dose Calculator
Safe Digoxin Dose Calculator
Recommended Dose
Critical Safety Information
This tool follows guidelines from the article: When starting amiodarone, cut digoxin dose by 50% immediately. For kidney impairment, reduce further to 1/3 of original dose.
Never adjust medication without medical supervision. This calculation is for educational purposes only.
Why This Drug Pair Can Be Deadly
Take two common heart medications - digoxin and amiodarone - and put them together, and you’ve got a recipe for disaster. Not because they don’t work, but because they work too well when combined. Digoxin, a drug used for decades to treat heart failure and irregular heartbeats, has a razor-thin safety margin. Its therapeutic level? Just 0.5 to 0.9 nanograms per milliliter in the blood. Go above that, and you risk poisoning. Go below, and it doesn’t help. Amiodarone, a powerful antiarrhythmic, is even more complex. It stays in your body for months, sometimes over a year, after you stop taking it. When these two drugs meet, digoxin levels can jump by 100% or more. That’s not a small change. That’s a trip to the ICU.
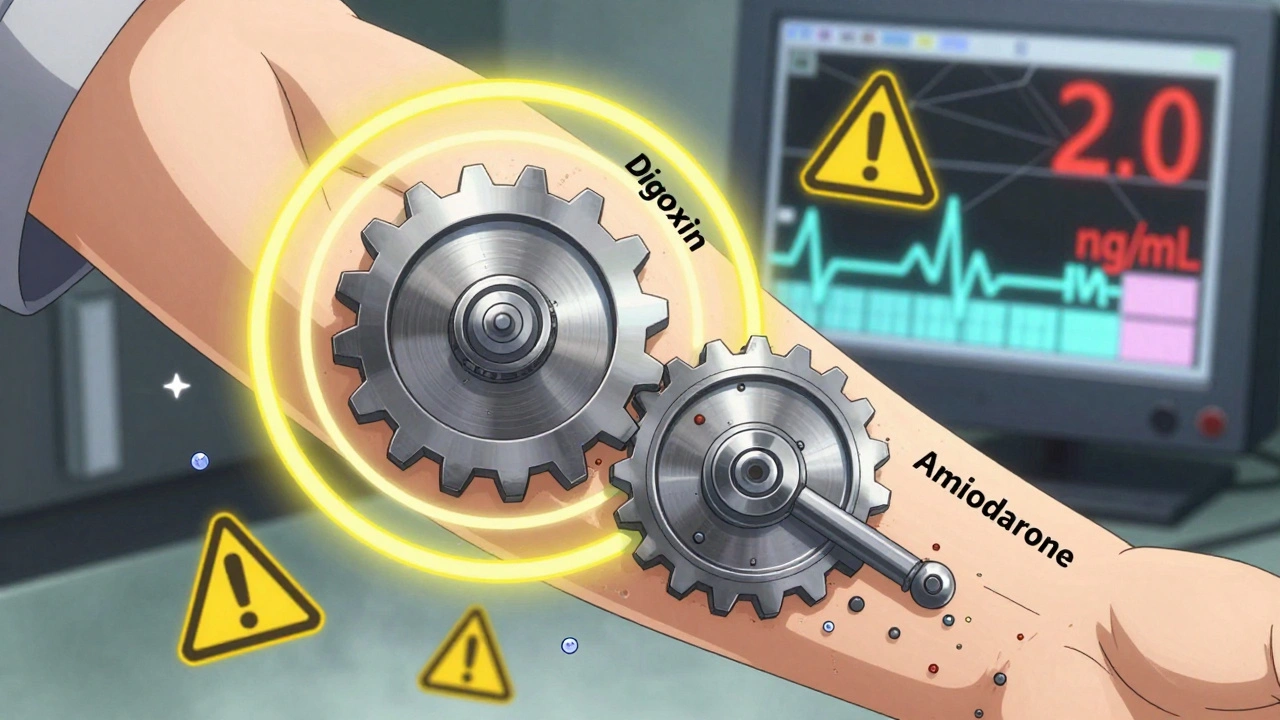
How the Interaction Actually Works
This isn’t just a guess. It’s been proven in labs, hospitals, and patient records since the 1980s. Amiodarone blocks a protein called P-glycoprotein - the body’s natural pump that kicks digoxin out of cells. When that pump gets clogged, digoxin builds up like traffic on a highway with no exits. At the same time, amiodarone slows down how fast the liver and kidneys clear digoxin. The result? Digoxin sticks around longer and piles up higher than it ever should. Studies show serum levels rise from safe averages of 0.97 ng/mL to dangerous levels near 2.0 ng/mL - more than double the upper limit. One 2020 study even found digoxin exposure increased by 40% to 60% when taken with amiodarone. That’s not a side effect. That’s a pharmacological collision.
What Happens When Toxicity Strikes
High digoxin levels don’t just cause nausea or dizziness. They trigger real, life-threatening chaos. The heart starts misfiring - slow rhythms, skipped beats, even ventricular tachycardia. Patients report blurred vision with yellow or green halos - a classic sign called xanthopsia. Electrolytes go haywire, especially potassium. One documented case in a 72-year-old woman showed potassium levels skyrocketing to 6.8 mEq/L (normal is 3.5-5.0). She needed ICU care for four days. Another study found that when doctors didn’t reduce digoxin doses after starting amiodarone, 35% of heart failure patients died within 30 days - up from just 8%. That’s a 27-point absolute increase in death risk. And it’s entirely preventable.
Why Doctors Still Miss This
You’d think with decades of research, everyone would know to adjust the dose. But they don’t. A 2022 study across 15 U.S. hospitals found only 44% of patients had their digoxin dose cut when amiodarone was added. In community hospitals, it was worse - nearly 7 out of 10 patients got the wrong dose. Why? Because the interaction is delayed. Digoxin levels don’t spike right away. They creep up over days, even weeks. By the time a patient feels sick, the doctor might not connect it to the new drug. And because amiodarone lasts so long - its half-life can be over 50 days - the danger doesn’t disappear when you stop it. The metabolite, desethylamiodarone, keeps blocking P-glycoprotein for up to two months. So even if you stop amiodarone, digoxin stays toxic.
The Only Safe Way to Manage It
There’s no room for guesswork. The guidelines are clear and consistent. When you start amiodarone, immediately cut the digoxin dose in half. That’s it. No waiting. No testing first. Just reduce it by 50% on day one. Why? Because by the time you get a blood level back, it’s already too late. The rise happens fast enough to cause harm before you can react. For patients with kidney problems - and most elderly patients do - cut it even further: down to one-third of the original dose. Check digoxin levels 72 hours after starting amiodarone. If levels are still climbing, reduce again. Repeat every few days until stable. At the University of Michigan, they made this protocol mandatory. Toxicity cases dropped from 12.3% to 2.1%. That’s not luck. That’s systems working.
Who’s at Highest Risk?
This isn’t a problem for everyone. It’s concentrated. Older adults - especially over 75. People with kidney disease. Those with low body weight. Patients already on multiple heart meds. In the U.S., about 1.2 million people have both atrial fibrillation and heart failure. Roughly 1 in 3 gets amiodarone. Nearly 1 in 4 gets digoxin. That means over a million people are walking around with this ticking clock in their bloodstream. The Veterans Health Administration cut digoxin toxicity by 41% just by adding an EHR alert that pops up when both drugs are prescribed together. Simple. Effective. Why isn’t every hospital doing this?
What’s Changing in Guidelines
The tide is turning. New guidelines from the European Society of Cardiology in 2024 now recommend avoiding digoxin entirely if you’re going to need amiodarone. Instead, use beta-blockers or calcium channel blockers for rate control. Why? Because digoxin’s risks now outweigh its benefits in most cases. Even the DIG trial, a major study from the 1990s, was reanalyzed in 2023 and showed a 38% higher death rate in patients taking both drugs - especially if their kidney function was already low. Digoxin prescriptions in the U.S. have dropped 18% since 2015. It’s not because the drug is obsolete. It’s because we’ve learned how dangerous it is in combination with common antiarrhythmics. The future is avoiding the combo altogether.

What to Do Right Now
If you’re on digoxin and your doctor adds amiodarone - don’t wait. Ask: "Are we reducing my digoxin dose?" If they say "We’ll monitor levels first," push back. By the time the lab results come back, you could already be toxic. If you’re on amiodarone and start feeling nauseous, seeing halos around lights, or your heart feels off - get a digoxin level checked immediately. And if you’ve stopped amiodarone in the past six weeks? Don’t assume the risk is gone. Your body still has the metabolite active. Any digoxin you take now is still at risk. This interaction doesn’t turn off like a light switch. It fades slowly. You have to plan for that.
What’s Next in Research
There’s a clinical trial underway right now - the DIG-AMIO trial - testing whether reducing digoxin by 33% instead of 50% is safer for patients with kidney issues. Results are expected in late 2025. But until then, stick with the proven path: cut it in half. No exceptions. No delays. No "we’ll see how they do." This isn’t theoretical. It’s happened too many times. Real people. Real deaths. Preventable ones.
Can I just lower my digoxin dose on my own if I start amiodarone?
No. Never adjust your digoxin dose without medical supervision. Even though guidelines say to cut it by 50%, your exact dose depends on your age, kidney function, weight, and other medications. A pharmacist or cardiologist should calculate your new dose and monitor your levels. Self-adjusting can lead to underdosing (which makes the drug useless) or overdosing (which can kill you).
How long does the interaction last after stopping amiodarone?
The interaction can persist for up to two months after you stop amiodarone. That’s because its main active metabolite, desethylamiodarone, has a half-life of 40-60 days. Even if you feel fine, your body is still blocking digoxin clearance. If you’re restarted on digoxin after stopping amiodarone, assume the interaction is still active unless your doctor confirms otherwise with a blood test.
Are there safer alternatives to digoxin when using amiodarone?
Yes. Beta-blockers like metoprolol or calcium channel blockers like diltiazem are preferred for heart rate control in atrial fibrillation when amiodarone is needed. They don’t interact dangerously with amiodarone and have better safety profiles. Digoxin is now considered a second-line option - only used when other drugs aren’t tolerated or are contraindicated, especially in heart failure patients with reduced ejection fraction.
Can I take amiodarone if I’ve had digoxin toxicity before?
It’s possible, but only under strict supervision. If you’ve had digoxin toxicity in the past, your risk is much higher. Your doctor will likely avoid digoxin entirely and use other rate-control medications. If digoxin is absolutely necessary, you’ll need a much lower starting dose, frequent blood tests, and close monitoring for signs of toxicity - including daily heart rhythm checks and electrolyte panels.
Why isn’t this interaction more widely known among patients?
Because it’s rarely explained. Most patients get a prescription and are told to take it - not warned about hidden dangers. Drug labels mention the interaction, but they’re written for doctors, not patients. Many patients don’t know they’re on digoxin at all. If you’re on either drug, ask your pharmacist: "Are there any dangerous combinations I should avoid?" That one question could save your life.
Final Takeaway
This isn’t a rare edge case. It’s a routine, preventable tragedy. Every time a doctor prescribes amiodarone without cutting digoxin, they’re gambling with someone’s life. The data is clear. The protocols are simple. The cost of inaction? Death. The solution? Cut the dose. Monitor closely. Avoid the combo if you can. That’s not just good medicine. It’s basic responsibility.
Man i read this and thought my grandpa almost died from this exact thing last year. Docs just threw amiodarone at him for afib and never touched his digoxin. He got dizzy, saw yellow circles, almost went into full arrest. Took his daughter screaming at the hospital to get them to check levels. Now he’s on metoprolol and fine. This needs to be screamed from rooftops.
Typical American medical negligence. In India we’ve known this since the 90s. We don’t wait for lab results-we cut the dose before the first pill is swallowed. Your system is broken. You rely on reactive medicine instead of proactive protocol. This isn’t science-it’s negligence dressed in white coats.
Just had a patient on this combo last week. We cut digoxin by 50% on day one, checked levels at 72 hours-up to 1.8 ng/mL. Cut again to 1/3. By day 5, down to 0.7. No ICU. No drama. Just following the damn guidelines. Why is this even a debate? It’s not rocket science. It’s basic pharmacokinetics.
This isn’t just a drug interaction-it’s a systemic failure. Imagine a bridge inspector who waits for the first car to crash before tightening the bolts. That’s what we’re doing here. We’re not just failing patients-we’re gambling with their lives using a loaded dice. And the worst part? The fix costs nothing. No new tech. No fancy app. Just a damn dose reduction. Why is that so hard?
Of course hospitals ignore this. They’re profit machines. Digoxin is cheap. Amiodarone is expensive. They’d rather kill a few old folks than lose revenue on a $0.02 dose adjustment. And don’t get me started on the EHR alerts-those are optional. Because why make life easier when you can make it lucrative?
Wait-so you’re telling me the FDA and every hospital in America didn’t know this? That’s not incompetence. That’s a cover-up. I’ve seen the patents. The manufacturers knew. They buried the data. Amiodarone’s maker? They had internal studies in 1998 showing 40% spike in digoxin levels. They didn’t warn anyone. They just kept selling. This is pharmaceutical murder. And they’re still doing it.
So let me get this straight-you’re saying the solution is to cut digoxin in half before checking levels… and you’re not even slightly worried about underdosing? What if the patient needs that full dose for their heart failure? You’re trading one risk for another like it’s a game of roulette.
Ohhh, here we go-the "cut it in half" crowd again. Let me guess-you also think we should just stop statins because some people get muscle pain? This isn’t a binary world. You reduce dose, you monitor, you titrate. You don’t just slash it like a barbarian with a cleaver. And for the love of God, stop pretending this is some revolutionary insight-it’s been in UpToDate since 2010.
As a British medic who’s seen this play out in NHS wards for decades-this is textbook. We’ve had protocols for this since the 1990s. The key isn’t just the dose reduction-it’s the culture. We train pharmacists to flag it. We mandate double-checks. We don’t rely on overworked doctors to remember every interaction. We build systems. Because when lives are on the line, hope isn’t a strategy.
Thank you for this. I work in a community clinic. We just implemented the 50% cut protocol last month. We’ve had zero toxicity cases since. One patient came in crying because she thought she was dying from "side effects"-turned out it was digoxin toxicity. She’d been on both drugs for 6 weeks. We changed her dose, she cried again-but this time from relief. This isn’t complex. It’s compassionate. And it’s long overdue.