Cholesterol Medication Comparison Tool
This tool helps you understand which cholesterol-lowering option might be best for your specific situation. Based on your inputs, it will recommend the most appropriate medication class and explain why.
Your Situation
Ezetimibe is a prescription medication that blocks the absorption of cholesterol from the small intestine, helping lower low‑density lipoprotein (LDL) levels. It’s often prescribed when statins alone aren’t enough or cause intolerable side effects.
Quick Takeaways
- Ezetimibe works by inhibiting intestinal cholesterol uptake, unlike statins which block liver synthesis.
- On average, ezetimibe cuts LDL by 15‑20% as monotherapy; combined with a statin, reductions can reach 35‑45%.
- Side‑effects are usually mild (headache, GI upset), and serious muscle issues are rare.
- Alternatives such as PCSK9 inhibitors, bile‑acid sequestrants, fibrates, and niacin each have distinct mechanisms and trade‑offs.
- Choosing the right therapy depends on baseline LDL, tolerance to drugs, cost, and cardiovascular risk.
Why Compare Ezetimibe with Other Lipid‑Lowering Drugs?
When a doctor orders a cholesterol‑lowering plan, patients often wonder whether ezetimibe is the best fit or if another option might work better. The answer isn’t one‑size‑fits‑all; it hinges on efficacy, safety, dosing convenience, and price. This guide walks you through the most common alternatives, laying out the pros and cons so you can have an informed conversation with your clinician.
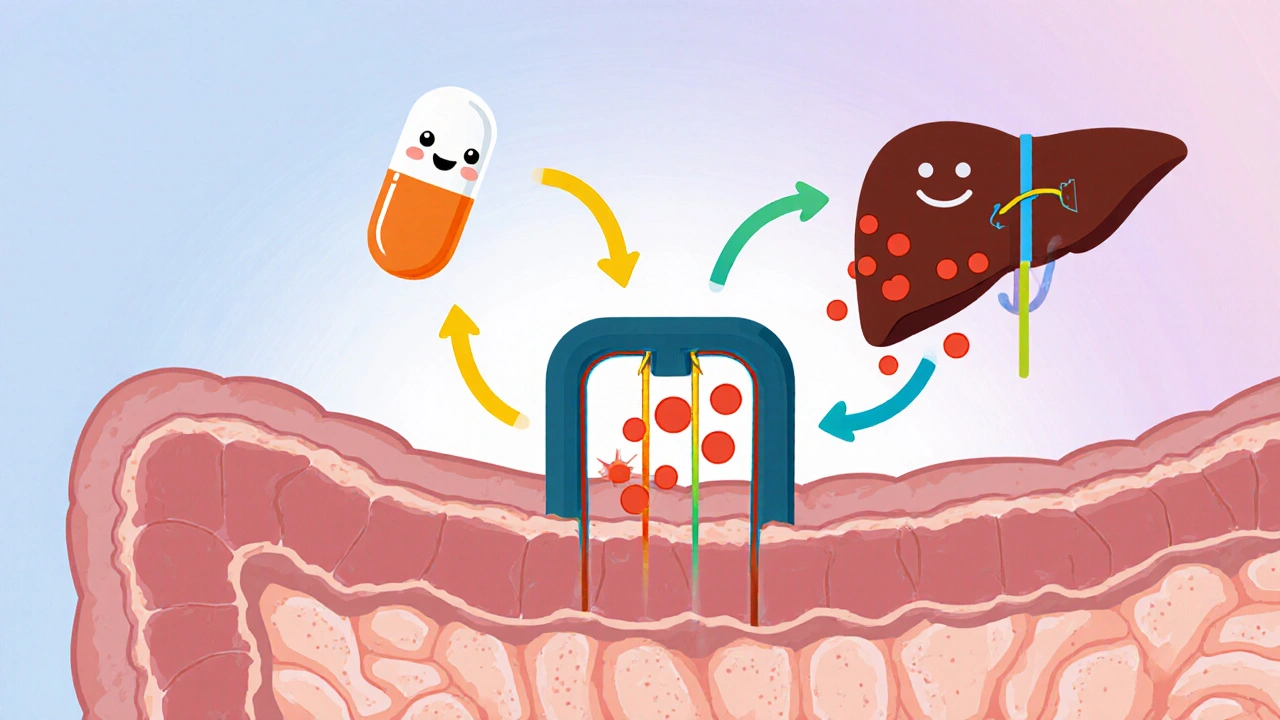
How Ezetimibe Works
The drug targets the Niemann‑Pick C1‑Like 1 (NPC1L1) protein on the brush border of intestinal cells. By blocking this transporter, ezetimibe prevents about 50% of dietary and biliary cholesterol from entering the bloodstream. The liver then pulls more LDL from circulation to meet its cholesterol needs, which drops blood LDL levels.
Major Alternatives at a Glance
Below are the most frequently prescribed alternatives. Each entry includes a brief definition, typical dose, LDL‑lowering potency, and key safety notes.
| Drug/Class | Mechanism | LDL Reduction | Typical Dose | Common Side‑Effects | Notable Points |
|---|---|---|---|---|---|
| Ezetimibe | Blocks intestinal NPC1L1 cholesterol absorption | 15‑20% alone; 35‑45% with statin | 10mg daily | Headache, mild GI upset | Low cost, few drug‑drug interactions |
| Statins | Inhibit HMG‑CoA reductase (liver cholesterol synthesis) | 20‑55% depending on potency | Varies (e.g., atorvastatin 10‑80mg) | Muscle pain, elevated liver enzymes | First‑line therapy; robust outcome data |
| PCSK9 Inhibitors | Monoclonal antibodies that increase LDL‑receptor recycling | 50‑60% (often >70% in high‑risk patients) | Alirocumab 75mg SC q2wks or Evolocumab 140mg SC q2wks | Injection site reactions, flu‑like symptoms | Highly effective; expensive; insurance‑driven |
| Bile‑Acid Sequestrants | Bind bile acids in gut, forcing liver to use cholesterol to make more | 10‑20% modest | Cholestyramine 4g daily (split doses) | Constipation, bloating, interference with absorption of other meds | Useful when statins intolerable; cheap; bland taste |
| Fibrates | Activate PPAR‑α, lowering triglycerides and modestly lowering LDL | 5‑15% LDL; 30‑50% TG | Fenofibrate 145mg daily | Gallstones, muscle issues (especially with statins) | Best for mixed dyslipidemia; not primary LDL tool |
| Niacin (Vitamin B3) | Reduces hepatic VLDL secretion, raises HDL | 10‑15% LDL; 15‑35% HDL increase | Extended‑release 1‑2g daily | Flushing, hyperglycemia, liver toxicity | Less used now; flushing mitigated with aspirin pre‑dose |
When Ezetimibe Shines
Because it works outside the liver, ezetimibe is a solid choice for patients who can’t tolerate high‑dose statins due to muscle pain or liver enzyme spikes. It also pairs nicely with a low‑to‑moderate statin, delivering a synergistic LDL drop without the need for a pricey injection.
Cost & Accessibility Considerations
Generic ezetimibe costs roughly $0.30‑$0.60 per tablet in the U.S., making it one of the most affordable non‑statin options. In contrast, PCSK9 inhibitors can run $1,400‑$1,600 per month before insurance offsets. Bile‑acid sequestrants sit at the low end, but the gritty texture can deter adherence.
Safety Profile: Who Should Avoid Ezetimibe?
Pregnant or breastfeeding individuals should only use ezetimibe if the benefits clearly outweigh risks, as data are limited. Patients with active liver disease are generally fine because ezetimibe isn’t metabolized heavily by the liver, but routine liver‑function monitoring is still recommended when combined with statins.

Putting It All Together: Decision‑Making Framework
Below is a quick decision tree you can discuss with your healthcare provider.
- Do you have astatin intolerance? - If yes, consider ezetimibe monotherapy or bile‑acid sequestrants.
- Is your LDL still >100mg/dL on maximally tolerated statin? - Add ezetimibe or consider a PCSK9 inhibitor for very high‑risk patients.
- Do you have high triglycerides (>200mg/dL) alongside LDL? - Fibrates or omega‑3 fatty acids may be added.
- Is cost a major barrier? - Generic ezetimibe or statins are budget‑friendly; PCSK9 inhibitors usually require prior‑auth.
Real‑World Example
John, 58, has a history of heart attack. He was on atorvastatin 40mg but developed persistent muscle aches. His cardiologist switched him to ezetimibe 10mg plus a reduced atorvastatin 10mg. Over 12 weeks, John’s LDL fell from 138mg/dL to 92mg/dL, and his muscle symptoms vanished. John avoided the high cost of a PCSK9 inhibitor while still hitting his target LDL.
Key Takeaway: No One‑Size‑Fit‑All
Whether you end up on ezetimibe alone, paired with a statin, or on a completely different class, the goal is the same-lower your LDL enough to protect your heart without unbearable side effects. Understanding each option’s mechanism, efficacy, safety, and cost lets you and your clinician tailor the best plan.
Frequently Asked Questions
Can I take ezetimibe with a statin?
Yes. Combining ezetimibe with a statin is a common strategy called “dual therapy.” It can boost LDL reduction by an extra 15‑20% compared to the statin alone, and most patients tolerate the combo well.
How long does it take to see LDL changes after starting ezetimibe?
LDL levels typically start dropping within 2‑4 weeks, with the full effect seen around 8‑12 weeks. Your doctor will likely repeat a lipid panel at the 3‑month mark.
Is ezetimibe safe for people with liver disease?
Because ezetimibe isn’t heavily processed by the liver, it’s generally safe for mild to moderate liver disease. However, doctors still monitor liver enzymes, especially if a statin is also used.
What are the main drawbacks of PCSK9 inhibitors compared to ezetimibe?
PCSK9 inhibitors are injections and cost significantly more than oral ezetimibe. Insurance approval can be a hurdle, and they’re usually reserved for patients at very high cardiovascular risk or those who can’t reach LDL goals with oral meds.
Can lifestyle changes replace ezetimibe?
Diet, exercise, and weight loss can lower LDL by 5‑15%, which helps but often isn’t enough for high‑risk patients. Medications like ezetimibe provide a predictable, measurable reduction that complements lifestyle work.
Sure ezetimibe is just a marketing ploy.
Ezetimibe can be a useful add‑on when statins aren’t enough. It’s inexpensive and easy to take, which makes adherence simpler. Combining it with a moderate‑dose statin often gets patients past the LDL target without stepping up to pricey injectables.
When you stare at the table of cholesterol‑lowering agents, you realize that each drug is a character in a grand drama of metabolic manipulation.
Ezetimibe, the shy understudy, slips into the gut and quietly blocks the NPC1L1 transporter.
Statins, the loud protagonists, roar in the liver, shutting down HMG‑CoA reductase.
PCSK9 inhibitors, the flamboyant heroes, march in as monoclonal antibodies, rescuing LDL receptors from degradation.
Bile‑acid sequestrants, the gritty side‑kicks, bind bile in the intestine and force the liver to burn cholesterol.
Fibrates, the modest poets, whisper to PPAR‑α, soothing triglycerides while modestly nudging LDL down.
Niacin, the old‑school sage, raises HDL and modestly lowers LDL, but its flush can be a theatrical firework.
In the real world, patients are the audience, and cost, side‑effects, and convenience dictate the encore.
Ezetimibe’s modest 15‑20% LDL drop as monotherapy can be the quiet applause that saves a heart.
When paired with a statin, the duet can slash LDL by up to 45%, a performance worthy of a standing ovation.
Yet the drug is cheap, a penny‑pincher’s delight, while PCSK9 inhibitors demand a fortune, turning the stage into a boutique.
Doctors must balance the script, considering liver function, muscle pain, and the patient’s wallet.
The guidelines suggest starting with a statin, then adding ezetimibe before resorting to injections.
Some clinicians, however, skip the statin altogether, fearing myalgia, and hand the patient ezetimibe as the lead.
The evidence shows that the combination reduces cardiovascular events, but the data are still unfolding.
In the end, the choice is personal, a narrative written between the doctor’s pen and the patient’s pulse.
It is noteworthy that ezetimibe offers a modest yet reliable reduction in LDL without imposing hepatic strain. Consequently, it warrants consideration for patients who experience statin intolerance.
One must wonder whether the pharmaceutical giants are quietly steering the narrative toward ever‑costlier biologics. Ezetimibe sits quietly in the shadows, perhaps because the profit motive favors the flashier injections.
Listen up, comrades! The drug cartel of cholesterol pills wants you to believe only the shiny, high‑priced PCSK9 monsters can save you, but the humble ezetimibe is the true patriot’s choice – cheap, effective, and un‑bowed by corporate greed.
While Kevin paints a vivid tableau of drug classes, the practical side of therapy often swims in the murky waters of insurance formularies. A physician may love the drama of PCSK9 heroes, yet the patient lives with a co‑pay that feels like a penalty. Ezetimibe, sitting quietly on the shelf, can be the unsung protagonist that actually gets taken. Moreover, adherence improves when the pill is small, cheap, and without the sting of injections. So, the clinical narrative should give the modest drug its rightful stage time.
Sure, ezetimibe is effective, but don’t let the glossy statin headlines blind you. It’s a solid, low‑key option that many overlook, and that’s exactly why it deserves a shout‑out 🙂
Cost matters more than hype.
Lisa’s reminder about formularies cuts to the bone of real‑world practice. The economics of care often dictate choice more than pharmacology textbooks. One must question whether our guidelines truly serve patients or the industry’s bottom line. The quiet efficacy of ezetimibe should be heralded, not hidden.
I’m fascinated by how each lipid‑lowering drug carries its own story. The balance between triglyceride control and LDL reduction can feel like walking a tightrope. Understanding these nuances helps us make smarter choices.
Mary, your observation hits the nail on the head; juggling TGs and LDL is indeed a delicate act. In practice, I’ve seen patients flip‑flop between fibrates and ezetimibe, chasing the perfect mix. The key is regular monitoring and being willing to adjust the regimen as the numbers shift. Patience and communication with your clinician become the safety net beneath that tightrope.
Let’s remember that lifestyle remains the foundation upon which any medication builds. Exercise, a Mediterranean diet, and smoking cessation amplify the benefits of ezetimibe and statins alike. A holistic approach ensures the best cardiovascular outcomes.
ezetimibe is ok if you cant take statins.
Indeed, the synergistic effect of ezetimibe with a low‑dose statin can be a game‑changer for many. It offers a realistic path to hitting LDL goals without overwhelming side‑effects.
While the holistic advice sounds noble, one has to ask who profits from the endless diet fads and fitness apps promoted by big corporations. The pharmaceutical push toward pricey biologics feels orchestrated, and ezetimibe’s modest profile is conveniently downplayed. Still, if a patient can’t afford the hype, the cheap pill remains the pragmatic choice. Trust your doctor, but keep an eye on the hidden agendas.