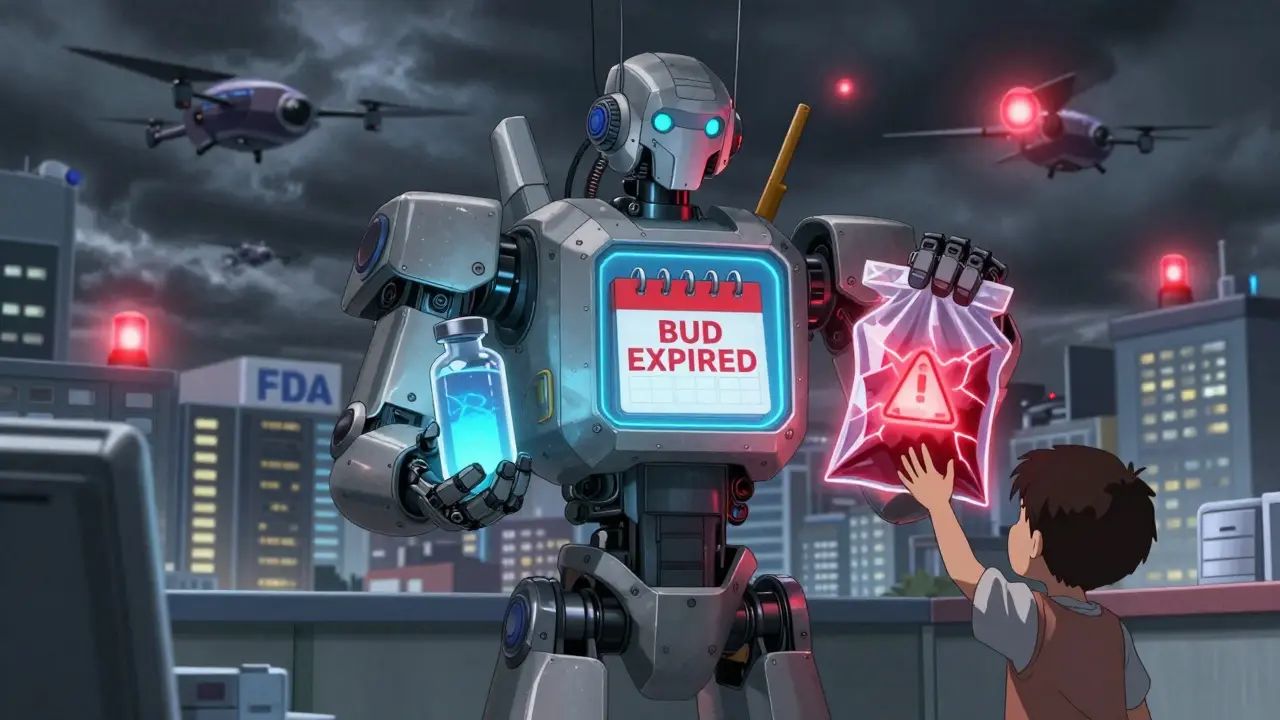
When you pick up a compounded medication, the label doesn’t say "expires on" like a regular prescription. Instead, it says "beyond-use date"-or BUD. If you don’t understand what that means, you could be taking a drug that’s no longer safe. Unlike factory-made pills with FDA-approved expiration dates, compounded medications are mixed by hand, often for very specific needs: allergies to dyes, rare dosages, or forms like liquids for kids who can’t swallow pills. But because they’re not mass-produced, they don’t get the same stability testing. That’s why the BUD matters more than you think.
What Exactly Is a Beyond-Use Date?
A beyond-use date is the last day a compounded medication is guaranteed to be safe and effective. It’s not a guess. It’s not a suggestion. It’s a scientifically determined cutoff based on how the specific mix of ingredients, container, and storage conditions will hold up over time. After this date, the drug might break down, lose strength, or even grow harmful bacteria. The USP <797> standard, which all U.S. compounding pharmacies must follow, defines it clearly: "the date after which a compounded preparation shall not be used."
Here’s the key difference: FDA-approved drugs get expiration dates from years of lab testing under strict conditions. Compounded meds? They get BUDs based on what the pharmacist can prove-through literature, manufacturer data, or direct testing. If the pharmacist doesn’t do the work, the BUD could be wrong. And that’s dangerous.
Why BUDs Are Not the Same as Expiration Dates
Think of expiration dates like a car’s factory warranty. The manufacturer tested every part under hundreds of conditions and said, "This will work for 5 years." BUDs are more like a homemade meal you put in the fridge. You know it’s fresh today, but how long will it last? It depends on the ingredients, the container, and whether it’s kept cold.
Take a simple example: a pain relief cream made by mixing a prescription drug with a base cream. The drug might be stable for years in its original tablet form. But once it’s blended into a cream, exposed to air, and stored in a plastic tube, it can degrade faster. A 2021 study showed that changing the pH of a compounded liquid made it break down 3.7 times faster than the commercial version. That’s why you can’t just copy the expiration date from the original bottle.
And containers matter. A syringe isn’t designed to store medicine long-term. Yet, 41.3% of retail pharmacies still assign BUDs to syringe-stored meds using data from vials. That’s like using a plastic grocery bag to store gasoline-technically it holds it, but it’s not safe.
How Pharmacists Determine BUDs (The Real Process)
Assigning a BUD isn’t just looking up a number. It’s a five-step science project. Here’s how it actually works:
- Identify every ingredient-including the active drug, solvents, preservatives, and even the dye. Even small changes affect stability.
- Classify the risk level-USP <797> divides compounded meds into low, medium, and high risk. Low-risk (like a simple saline flush) might get a 48-hour BUD at room temperature. High-risk (like an IV bag with antibiotics) might only last 24 hours.
- Check the manufacturer’s data-if the original drug came with stability info, that’s a starting point. But only if the formulation hasn’t changed.
- Consult validated literature-there are databases with over 14,000 tested compounded formulas. But only 29.4% of pharmacists use them regularly.
- Test it-the gold standard. High Performance Liquid Chromatography (HPLC) can measure how much active ingredient remains over time. But only 37.2% of compounding labs use properly validated HPLC methods.
Most pharmacists rely on steps 1-4. That’s risky. A 2022 analysis found that 12.7% of medication errors with compounded drugs came from incorrect BUDs. And in 68% of those cases, the error was because the pharmacist didn’t account for the container or how the ingredients interacted.

What Happens When BUDs Are Ignored?
In 2021, the FDA recalled 1,247 compounded sterile products from one pharmacy because they were contaminated with bacteria. Why? The BUD had been stretched too far. The meds were stored in plastic bags instead of glass vials. The temperature wasn’t controlled. The pharmacist assumed the BUD could be the same as a commercial product. People got sick.
It’s not just contamination. Degradation is silent. A painkiller that’s lost 20% of its strength won’t feel different to the patient. But it won’t work. A hormone therapy that breaks down into toxic byproducts? That’s a long-term risk no one talks about.
And enforcement is tightening. In 2023, BUD violations jumped to 34.1% of all compounding citations-up from 28.6% the year before. The FDA is watching. States are auditing. Pharmacies are being fined.
How to Know If Your BUD Is Safe
If you’re the patient, you can’t run HPLC tests. But you can ask smart questions:
- "Is this BUD based on testing, or just a guess?"
- "What’s the risk level of this preparation?"
- "Was it stored in the right container?"
- "Does the pharmacy have a stability testing program?"
Ask for the documentation. By law, pharmacies must keep written proof of how they assigned the BUD. If they can’t show it, be cautious. Hospitals follow strict rules-92.4% compliance. Retail pharmacies? Only 76.8%. That gap matters.
Also, check the storage instructions. If the label says "refrigerate," and you left it on the counter for three days? The BUD is invalid. Temperature swings are one of the biggest killers of compounded meds.
The Future: More Compounding, More Risk
Personalized medicine is growing fast. By 2030, nearly 1 in 5 prescriptions could be compounded. That means more BUDs. More chances for error. That’s why USP is pushing new rules: starting in 2024, any BUD longer than 30 days will require direct stability testing. That’s a big shift. Right now, 23.7% of compounded meds have BUDs longer than that-based on literature alone.
Some pharmacies are using new tech. SmartBUD systems monitor real-time temperature and light exposure. One pilot showed a 47% drop in BUD errors. That’s promising. But tech won’t fix bad training. Pharmacists need 120 hours of specialized education just to get this right.
Bottom Line: Don’t Assume, Ask
A beyond-use date isn’t a marketing label. It’s a safety boundary. And if it’s not backed by science, it’s just a number on a sticker. Whether you’re a patient, a caregiver, or a health professional, treat every BUD like a live wire. Don’t use it after the date. Don’t stretch it. Don’t guess. And if you’re unsure-ask for the proof. Your health depends on it.

So let me get this straight-you’re telling me some pharmacist in a basement with a hot glue gun and a calculator just guesses how long my weird hormone cream will last? And I’m supposed to trust that? I’ve seen pharmacies use yogurt containers for IV bags. This isn’t medicine, it’s Russian roulette with a side of aspirin.
And don’t even get me started on the ‘literature-based’ BUDs. That’s like using a 1998 Ford manual to fix a Tesla. Half the time, the ‘study’ they’re quoting was done on a different solvent, in a different climate, by someone who probably failed organic chemistry.
My cousin took a compounded pain cream that ‘expired’ in 30 days. She used it for six months. Got a skin infection. The pharmacy said ‘oops, our bad.’ No apology. No refund. Just a pamphlet on ‘medication safety.’
Someone needs to burn down a few of these labs. Or at least make them wear lab coats with warning labels.
Also, why is this even legal? The FDA lets this fly? I’m moving to Canada.
i never knew budes were so complicated. i always thought if it looks fine and smells okay, its fine. but now i realize-its not about looks. its about chemistry. and trust. and how much the pharmacist actually cares.
in india, we dont even have proper compounding labs in most towns. people just mix stuff from different bottles and call it a day. sometimes they use tap water. i shudder.
but also… isnt this the same with a lot of medicine? we trust the system until it fails us. maybe the real issue isnt the bud-it’s that we dont question enough.
thanks for making me think. i’ll ask my pharmacist next time. even if he rolls his eyes.
the concept of beyond-use date is deeply human. we want certainty in a world that offers none. we cling to dates like prayer beads, hoping they’ll shield us from chaos.
but stability is an illusion. even factory pills degrade. even glass shatters. even the best science is just a snapshot of time.
perhaps the real question isn’t how long the medicine lasts-but how long we’re willing to pretend we control nature.
the pharmacist is not a magician. just a man with a scale and a prayer.
and yet-we still trust him.
is that faith? or folly?
As a healthcare professional from India, I must commend this detailed and accurate breakdown. Compounded medications are indeed a lifeline for patients with unique needs-but they demand the highest standards of practice.
In our country, we see similar challenges: lack of training, outdated guidelines, and pressure to cut corners. But I’ve seen pharmacies in Delhi and Bangalore implement full HPLC testing and digital BUD tracking-and the results are transformative.
Education is the key. Pharmacists need mandatory certification in compounding stability. Regulatory bodies must enforce compliance-not just issue fines after people get sick.
Let’s not wait for another FDA recall. Let’s build a culture of excellence, not just compliance.
And patients: your questions are not annoying. They’re necessary. Keep asking.
Man, I had no idea this was such a mess. I’ve had a few compounded prescriptions-mostly for my kid’s allergy meds-and never thought twice. Just trusted the label.
Now I’m kinda freaked out. I’ll be asking my pharmacist all those questions next time. Honestly, I think I’ll even ask to see the documentation. Feels weird to do that, but… better safe than sorry.
Also, the part about plastic bags for IVs? That’s wild. I bet most people have no clue. This should be on the news.
Thanks for the heads-up. Really appreciated.
Oh wow. So America’s healthcare system is now run by people who think a ‘study’ from 2007 is enough to justify putting a 90-day BUD on a liquid antibiotic stored in a Ziploc.
And we wonder why people die.
At least in the UK, we have actual pharmacists with degrees who don’t outsource stability testing to a guy named Dave who works the night shift at CVS.
But hey, at least your BUDs come with cute little stickers. That’s something, right?
Wow. I just spent 20 minutes reading this like it was a thriller novel. And honestly? It should be.
Let’s be real-this isn’t just about chemistry. It’s about power. Who gets to decide what’s safe? Why are we trusting a system that admits 70% of pharmacists don’t use the databases? Why is HPLC considered ‘gold standard’ but only used by a third of labs?
And yet… I still took my compounded thyroid med past the BUD. Twice.
Because I’m tired. Because I’m broke. Because I thought, ‘it’s probably fine.’
So maybe the real problem isn’t the pharmacist.
It’s us.
We’re the ones who don’t ask. We’re the ones who don’t push back. We’re the ones who say ‘it’s fine’ when it’s not.
And now I feel guilty.
Also, typo: ‘budes’ not ‘buds.’ But you get it.
Let’s be clear: this entire post is a fearmongering piece dressed up as public service. Yes, there are bad actors. But 12.7% of errors? That’s less than 1 in 8. Meanwhile, FDA-approved drugs have a 2.5% error rate in dosing alone. And they’re mass-produced.
You’re ignoring the fact that compounded meds save lives daily-children with rare metabolic disorders, cancer patients with severe allergies, elderly with swallowing issues. Without them, many would die.
The system isn’t perfect. But it’s not a horror story. It’s a necessary compromise. And the FDA’s crackdowns are mostly targeting small pharmacies while letting big corporate compounding labs off the hook.
Stop scaring people. Start demanding accountability across the board-not just for the underdogs.
Also, ‘ask for proof’? That’s not a patient’s job. It’s the pharmacist’s responsibility to provide it. You’re shifting blame.