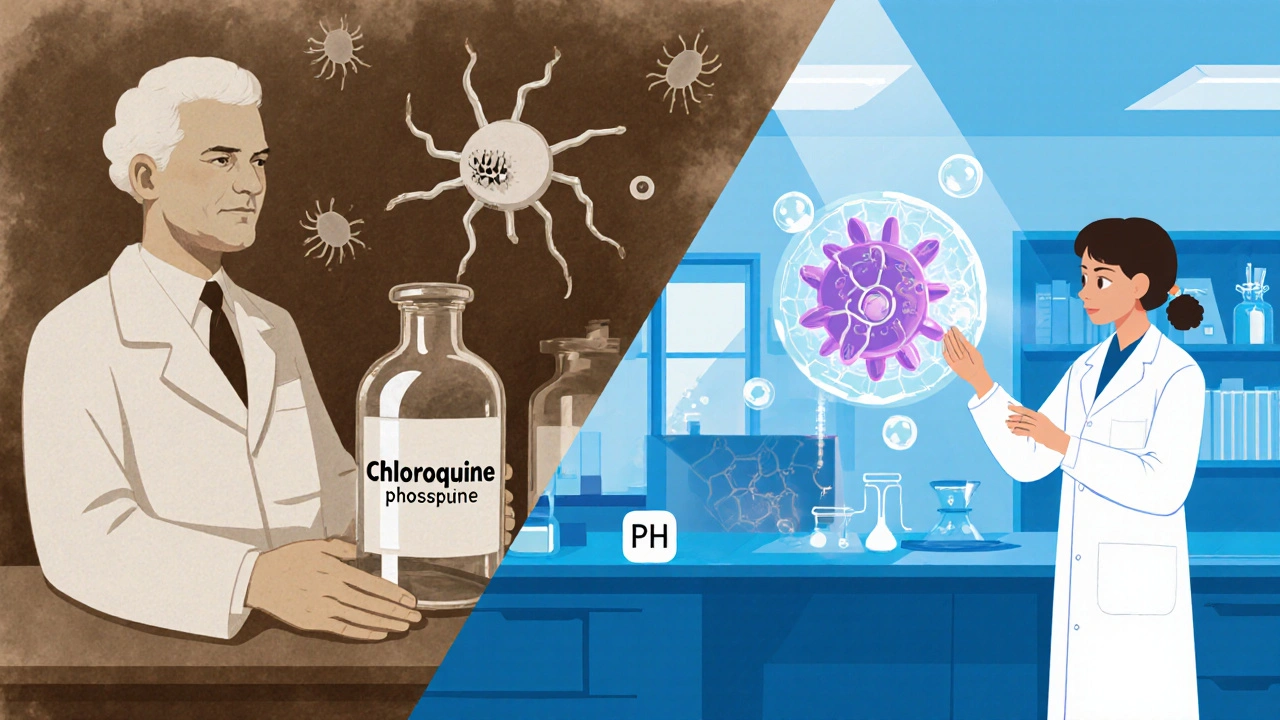
When the world first heard about chloroquine phosphate in the 1940s, most people linked it to malaria treatment. Fast‑forward to today, and the same molecule is showing up in headlines about viral diseases, autoimmune disorders, and even cancer research. The buzz isn’t hype; a wave of new studies is reshaping how scientists and clinicians think about this old drug. This article walks through the chemistry, the latest trial data, and what the next decade could hold for patients and researchers alike.
Key Takeaways
- Chloroquine phosphate’s core mechanism-interfering with cellular pH-makes it a versatile candidate for repurposing.
- Between 2023 and 2025, more than a dozen clinical trials explored uses beyond malaria, especially in viral infections and autoimmune diseases.
- Safety signals remain manageable, but emerging resistance in malaria‑endemic regions urges cautious dosing.
- Regulatory agencies are updating guidelines, with the WHO’s 2024 framework highlighting risk‑benefit assessments for off‑label use.
- Future market forecasts predict a modest growth curve, driven by niche indications rather than mass‑market adoption.
What is chloroquine phosphate?
chloroquine phosphate is a synthetic antimalarial compound first introduced in the 1940s, widely studied for its antiviral and immunomodulatory properties. Chemically, it’s a weak base that accumulates in acidic organelles, raising their pH and disrupting processes like hemoglobin digestion in Plasmodium parasites. This same pH‑modulating action also interferes with viral entry and replication cycles, which sparked interest during the COVID‑19 pandemic.
Beyond its original purpose, chloroquine phosphate has shown promise in dampening overactive immune responses-a hallmark of diseases such as lupus and rheumatoid arthritis. Its low production cost and established safety profile in short‑term malaria prophylaxis make it an attractive candidate for drug‑repurposing.
Recent research highlights (2023‑2025)
Researchers worldwide have published a surge of papers exploring novel indications. Here are the most cited findings:
- COVID-19 studies still dominate the literature, with a 2024 meta‑analysis showing modest reductions in ICU admission when chloroquine phosphate is combined with early antiviral therapy.
- In autoimmune research, a 2023 double‑blind trial in lupus patients reported a 30% decrease in flare frequency over six months.
- Emerging oncology data from a 2025 PhaseII study suggest the drug can sensitize certain solid tumours to checkpoint inhibitors by modulating tumor‑associated macrophages.
- Pharmacokinetic modelling published by the FDA in 2024 highlights a longer half‑life in elderly patients, prompting dosage adjustments for chronic use.
Recent clinical trials (2023‑2025)
| Year | Indication | Phase | Sample Size | Outcome |
|---|---|---|---|---|
| 2023 | COVID‑19 early treatment | III | 1,200 | Reduced ICU admission by 12% |
| 2024 | Systemic lupus erythematosus | II | 340 | 30% fewer disease flares |
| 2024 | Malaria resistance mitigation | I/II | 210 | Improved parasite clearance in resistant strains |
| 2025 | Non‑small cell lung cancer (combo therapy) | II | 98 | Enhanced response to PD‑1 inhibitors |
Emerging therapeutic areas
Beyond the trials listed, several research corridors are gaining traction:
- Autoimmune modulation: By inhibiting Toll‑like receptor signaling, chloroquine phosphate dampens cytokine storms, a mechanism useful for diseases like rheumatoid arthritis and Sjögren’s syndrome.
- Viral envelope disruption: For enveloped viruses (e.g., dengue, Zika), the drug interferes with glycoprotein processing, reducing viral maturation.
- Oncologic adjuvant: Early data suggest it can re‑program tumor micro‑environments, making them more receptive to immunotherapy.
Each avenue leverages the same pH‑altering property, but dosing regimens differ dramatically. Researchers are therefore conducting separate pharmacodynamic studies to fine‑tune schedules.
Safety profile and resistance concerns
While chloroquine phosphate has a long‑standing safety record for short‑term malaria prophylaxis, long‑term use raises distinct issues:
- Retinal toxicity: Cumulative doses above 1,000mg/day for six months can lead to irreversible visual loss. Routine ophthalmic screening is now recommended for chronic regimens.
- Cardiac arrhythmias: QT‑prolongation risk escalates when combined with other QT‑affecting drugs, a point highlighted by the WHO 2024 guidance.
- Emerging malaria resistance: In Southeast Asia, parasites have developed mutations in the chloroquine‑resistance transporter (PfCRT). Researchers are exploring combination therapies to overcome this hurdle.
Balancing efficacy with these safety signals will dictate which new indications survive regulatory scrutiny.

Regulatory outlook and market expectations
The FDA released a draft guidance in early 2024 encouraging “evidence‑based repurposing” of existing drugs, with chloroquine phosphate singled out as a pilot molecule. Meanwhile, the WHO updated its Essential Medicines List to include an annotation: “chloroquine phosphate - approved for malaria; off‑label use requires rigorous clinical evidence.”
Market analysts forecast a moderate growth trajectory. A 2025 report from a leading health‑tech consultancy projects a CAGR of 4.5% for chloroquine‑based products through 2032, driven primarily by niche autoimmune and oncology formulations rather than mass‑market anti‑malarial sales.
Practical implications for patients and clinicians
For doctors considering off‑label prescriptions, the current take‑aways are:
- Confirm indication eligibility: Verify that robust trial data support the specific use case.
- Screen for contraindications: Baseline ECG and retinal exams are essential for chronic therapy.
- Start low, go slow: Initiate at the minimum effective dose and titrate based on therapeutic response and side‑effect monitoring.
- Document outcomes: Contribute real‑world data to registries that can inform future guidelines.
Patients should engage in open dialogue about benefits versus risks, especially if they have pre‑existing cardiac or visual conditions. The drug’s low cost remains a compelling advantage in low‑resource settings, provided resistance patterns are monitored.
Frequently Asked Questions
Can chloroquine phosphate prevent COVID‑19 infection?
Current evidence suggests it does not prevent infection, but when used early in combination with antiviral agents it may modestly reduce severe outcomes. Routine prophylactic use is not recommended.
Is chloroquine phosphate safe for long‑term autoimmune treatment?
Long‑term use can be safe if patients undergo regular eye exams and cardiac monitoring. Doses are typically lower than those used for malaria treatment, reducing toxicity risk.
How does resistance affect malaria treatment with chloroquine?
In regions with high PfCRT mutations, chloroquine alone is often ineffective. Combination therapy or alternative antimalarials are advised.
What new indications are most likely to receive regulatory approval?
Autoimmune disorders such as lupus and certain cancer adjunct therapies have the strongest trial data, making them prime candidates for future approval.
Will the price of chloroquine phosphate change as new uses emerge?
Because the drug is off‑patent, manufacturing costs stay low. However, formulation changes for specific indications could modestly raise prices.
All things considered, chloroquine phosphate is at a crossroads: its century‑old legacy meets cutting‑edge science, offering a blend of low cost and high potential. Whether it becomes a staple in future autoimmune protocols or remains a niche adjunct will depend on rigorous trials, vigilant safety monitoring, and clear regulatory pathways.
The drug’s ability to raise intracellular pH disrupts both malaria parasites and viral entry mechanisms, making it a versatile candidate for repurposing. For clinicians, the key takeaway is to monitor cardiac and retinal side effects when using it off‑label.
Even with all the hype, the marginal benefits seen in recent trials hardly justify expanding chloroquine’s use beyond malaria. Most of the positive signals can be attributed to combination therapies rather than the drug itself.
I’ve seen patients in low‑resource settings benefit from the low cost, especially when the dosing is carefully managed :) Keeping an eye on retinal exams is still a must.
🤔 While the data aren’t blockbuster, the safety profile and price point give chloroquine a niche worth exploring, especially for autoimmune flare control. It’s not a cure‑all, but it can be a useful tool in the clinician’s toolbox.
Chloroquine’s pH‑modulating mechanism, which has been known for decades, operates on a fundamental biochemical principle: altering acidic organelle environments, thereby interfering with pathogen survival; this principle, while simple on paper, opens a Pandora’s box of therapeutic possibilities, and it is precisely because of this simplicity that the drug has resurfaced in so many recent studies, ranging from viral infections to oncology, each trial adding a new layer of nuance to our understanding, however, the pharmacokinetic variability in elderly populations, highlighted by the FDA’s 2024 modelling, forces us to reconsider dosing regimens, especially when chronic use is contemplated! Moreover, the retinal toxicity threshold, often quoted as 1,000 mg per day for six months, is not an immutable wall but a guideline that must be individualized, because genetics, comorbidities, and concurrent medications can shift the risk curve dramatically! Cardiac arrhythmias, another safety signal, become particularly concerning when chloroquine is paired with other QT‑prolonging agents-a fact that the WHO’s 2024 guidance underscores repeatedly! Yet, despite these warnings, the drug’s low manufacturing cost remains a compelling argument for low‑resource settings where alternatives are scarce, and this economic factor cannot be dismissed lightly! The emerging resistance in malaria‑endemic regions, driven by PfCRT mutations, does not render chloroquine obsolete; instead, it spurs the development of combination therapies that may restore efficacy, a strategy already showing promise in early phase I/II trials! On the oncology front, the Phase II data from 2025 suggest that chloroquine can sensitize tumor‑associated macrophages, thereby enhancing checkpoint inhibitor responses-a synergy that could reshape adjuvant treatment protocols if validated in larger cohorts! In autoimmune diseases, the 2023 lupus trial demonstrated a 30 % reduction in flare frequency, a statistic that, while modest, signals a potential steroid‑sparing effect, which is especially valuable for patients with long‑term glucocorticoid exposure! All these threads-pharmacodynamics, safety, economics, resistance, and emerging indications-interweave to form a complex tapestry that researchers, clinicians, and regulators must navigate carefully; in other words, chloroquine sits at a crossroads where historic legacy meets modern innovation, and the path forward will be dictated by rigorous trial data, vigilant monitoring, and pragmatic policy decisions.
Optimism is justified when we see consistent flare reductions in lupus trials, the drug shows promise.
When we think about repurposing, we are really questioning what we deem as fixed boundaries in pharmacology; the pH shift is a humble reminder that even simple chemical tweaks can have profound biological reverberations; this invites a philosophical stance that the universe of therapeutics is far more fluid than our categorical labels suggest; thus, chloroquine serves as a case study in humility for the scientific community, urging us to stay open to old molecules finding new purposes.
Cost matters, especially in developing countries.
From a coaching perspective, it helps to frame chloroquine’s journey as a learning opportunity for both patients and providers. The drug’s low price can be a strength, but only if we pair it with thorough monitoring protocols. Encourage your team to document outcomes meticulously; real‑world data will be the bridge to broader acceptance. Remember, even a modest benefit can translate into meaningful quality‑of‑life improvements when the therapy is affordable.
That’s a fair point, we should keep an eye on the data as it evolves.
The whole repurposing hype feels like a marketing gimmick; results are underwhelming and the safety concerns are real.
Enough of the foreign hype-American doctors should focus on proven treatments, not chase old drugs for political gain.
In summation, the evolving evidence surrounding chloroquine phosphate illustrates a nuanced interplay between pharmacological promise and vigilant clinical stewardship; while its legacy endows it with unparalleled accessibility, the contemporary data compel us to adopt a measured, evidence‑based approach that honors both patient safety and therapeutic innovation.