Every year in the U.S., over 107,000 people die from drug overdoses. Most of these deaths aren’t caused by one drug alone-they happen when multiple substances mix in dangerous ways. You might think you know what you’re taking, but street drugs are often laced with fentanyl. Prescription pills might be combined with alcohol or sleep aids you don’t even think of as risky. The truth is, drug interactions that increase overdose risk are silent killers-and they’re almost always preventable.
What Makes a Drug Interaction Deadly?
Not all drug interactions are the same. Some cause nausea or dizziness. Others can stop your breathing. The deadliest combinations involve substances that all slow down your central nervous system (CNS). These include opioids like oxycodone or heroin, benzodiazepines like Xanax or Valium, alcohol, sleep meds like Ambien, and even some muscle relaxants. When these are taken together, they don’t just add up-they multiply. A 2022 study in JAMA Internal Medicine found that mixing opioids and benzodiazepines increases the risk of fatal overdose by more than 10 times. Alcohol mixed with opioids raises the chance of respiratory depression by 67%. That means your body stops breathing before you even realize something’s wrong.Why Self-Reporting Fails
If you’ve ever been asked by a doctor, “Are you taking any other medications?” you’ve probably said no-even if you were taking Xanax for anxiety or drinking wine every night. Why? Because most people don’t think of those as “medications.” They think of prescriptions only. But 58% of patients underreport benzodiazepine use, and 68% of people prescribed opioids say they were never asked about alcohol or other drugs. A Reddit user who works in emergency medicine shared that in 12 years, she saw 217 overdose cases where patients denied using benzodiazepines-until after naloxone was given. Then, 82% admitted they’d been mixing them with opioids. The problem isn’t dishonesty. It’s language. Asking “Are you taking other meds?” doesn’t trigger the right memories. Asking “Do you ever take medicines not prescribed to you?” increases honest answers by 52%, according to a 2022 study in Addiction. People need to feel safe, not judged.How Clinicians Check for Risk
Doctors and pharmacists use tools designed to catch these risks before they turn deadly. The CDC’s Opioid Risk Tool (ORT) is a five-question screening that takes less than two minutes. It doesn’t ask for a full list-it asks targeted questions like, “Have you ever used drugs or alcohol to cope with stress?” or “Have you ever been treated for substance use?” Pharmacists use the Beers Criteria, updated every two years by the American Geriatrics Society, to spot dangerous combinations in older adults. For example, mixing an opioid with an antihistamine like diphenhydramine (Benadryl) can be deadly for seniors because both depress breathing. The FDA’s Drug Interaction Checker and MedlinePlus are reliable for prescription and OTC drugs, but they miss something huge: street drugs.
The Gap: Illicit Drugs and Street Names
Digital tools can’t warn you if you’re taking “Molly” that’s actually fentanyl-laced powder. Or if “percocet” you bought online contains carfentanil. According to the National Harm Reduction Coalition, 73% of dangerous interactions involve drugs known by multiple street names. “Downers,” “benzos,” “sleepers,” “blues,” “yellow jackets”-these aren’t medical terms, but they’re what people use. That’s why harm reduction workers don’t ask about “medications.” They use cards with pictures or simple lists: “Have you used any of these in the last week?” with icons or names like heroin, fentanyl, Xanax, alcohol, cocaine, meth, benzodiazepines, sleep pills. A 2023 SAMHSA survey found that when outreach workers used this approach, disclosure rates jumped. People felt less like they were being interrogated and more like they were being helped. One user said, “My doctor asked specifically about ‘downers’ instead of just medications, so I admitted to using Valium with my oxycodone-she gave me naloxone and saved my life.”What You Can Do Right Now
You don’t need to be a doctor to protect yourself or someone you care about. Here’s how:- Ask yourself: “Have I taken anything not prescribed to me?” That includes pills from a friend, alcohol, sleep aids, or street drugs.
- Know the red flags: Mixing opioids with any depressant (alcohol, benzos, sleep meds) = high risk. Mixing stimulants like cocaine or meth with opioids is also dangerous-it masks overdose symptoms until it’s too late.
- Check your meds: Use the FDA’s Drug Interaction Checker or MedlinePlus. Enter every pill, patch, or liquid you take-even herbal ones like kava or kratom, which can depress breathing.
- Ask your pharmacist: When you pick up a new prescription, say, “Can you check this with everything else I take-even things I don’t think are drugs?”
- Carry naloxone: If you or someone you know uses opioids, alcohol, or benzodiazepines, have naloxone on hand. It can reverse an opioid overdose in minutes. It’s available without a prescription in most states.
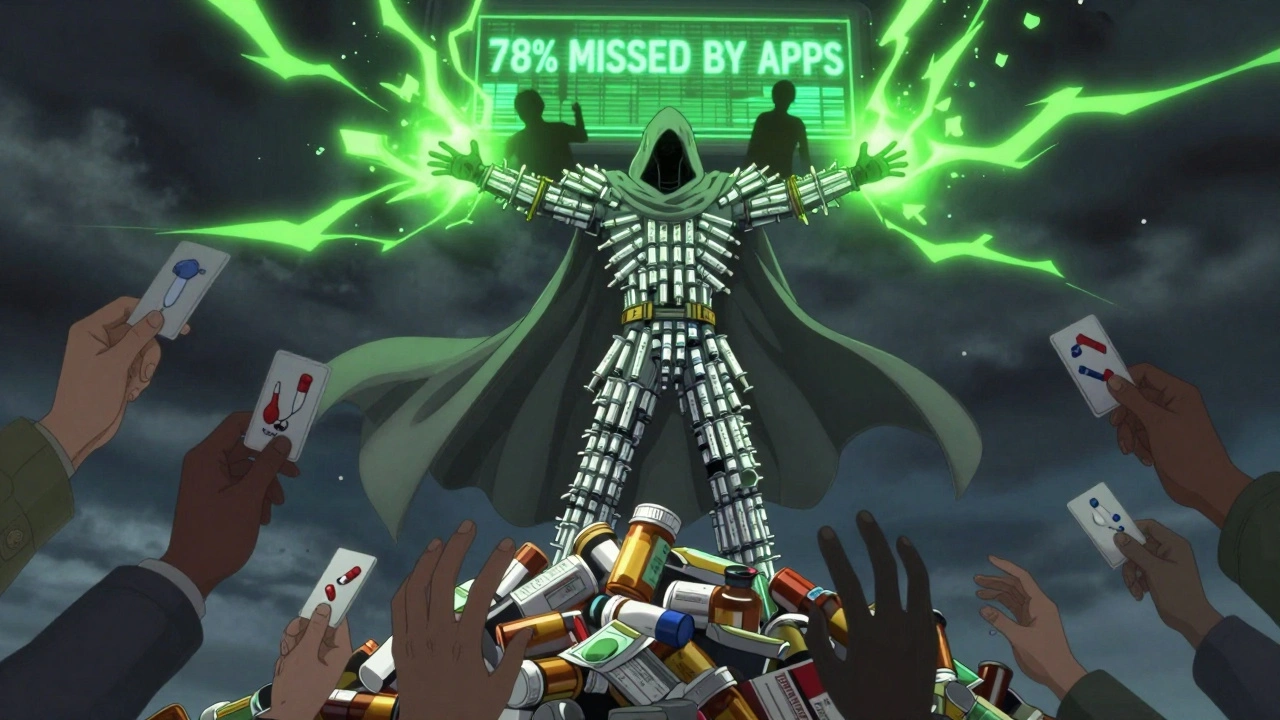
What’s Missing From Digital Tools
Even the best apps have blind spots. They don’t know if you shared a pill with a friend. They don’t know if your painkiller came from a stranger online. They don’t know if your “heroin” was cut with fentanyl. That’s why clinical guidelines now say: Always ask, even if the system says it’s safe. A 2023 study in JAMA Network Open found that digital tools miss 78% of dangerous interactions involving fentanyl analogs. The only way to catch those is through direct, non-judgmental conversation.Who Should Be Checking?
Everyone who prescribes, dispenses, or uses these substances should be involved. Doctors, nurses, pharmacists, peer support workers, and even friends and family can make a difference. In 2024, 63% of U.S. hospitals now ask about non-prescribed substances in overdose screenings-up from just 22% in 2019. But community programs still struggle. Only 17% of syringe service programs have access to pharmacists who can check for interactions. If you’re using drugs, you’re not alone. If you’re worried about someone else, don’t wait for them to ask for help. Start the conversation. Ask about what they’re really taking-not just what’s on a label.Resources You Can Use Today
- Overdose Risk Self-Check by the National Harm Reduction Coalition: A free, 10-question tool available in 12 languages. It’s validated to be 88% accurate.
- FDA Drug Interaction Checker: Updated monthly. Covers 1,200+ prescription and OTC drugs.
- MedlinePlus Drug Information: Run by the National Library of Medicine. Covers 10,000+ substances.
- Naloxone access: Available at most pharmacies without a prescription. Some community centers give it out for free.
The goal isn’t to scare you. It’s to give you power. Most overdose deaths aren’t accidents-they’re preventable. The tools exist. The knowledge exists. What’s missing is the conversation. Start yours today.
Can I check for drug interactions myself without a doctor?
Yes. Use free, trusted tools like the FDA’s Drug Interaction Checker or MedlinePlus. But remember: these only cover legal, named medications. They won’t warn you about street drugs like fentanyl-laced powder or unknown pills. For that, you need to ask yourself: Have I taken anything not prescribed? Have I mixed alcohol, sleep aids, or anxiety meds with painkillers? If yes, you’re at risk.
Are over-the-counter drugs safe to mix with opioids?
No. Many OTC meds can be dangerous. Cold and flu medicines often contain dextromethorphan or diphenhydramine-both depress the central nervous system. Mixing them with opioids increases the risk of breathing problems. Even herbal supplements like kava, valerian, or kratom can be risky. Always check with a pharmacist before combining anything with opioids.
Why do some people overdose even when they take the same dose they always have?
Tolerance drops fast. If you’ve been away from opioids for just 72 hours-whether due to jail, rehab, or stopping on your own-your body forgets how to handle the same dose. That’s why overdose risk spikes after periods of abstinence. It’s not about how much you take-it’s about how much your body can still handle. Always start low if you’re returning after a break.
Is naloxone only for heroin overdoses?
No. Naloxone reverses overdoses caused by any opioid, including prescription painkillers, fentanyl, and counterfeit pills. It does not work on alcohol, benzodiazepines, or stimulants like cocaine or meth. But since most overdoses involve multiple drugs, naloxone is still critical. If someone is unresponsive, not breathing, or turning blue, give naloxone anyway-it won’t harm them if opioids aren’t involved.
Can I get naloxone without a prescription?
Yes. In all 50 U.S. states and many other countries, naloxone is available without a prescription at pharmacies. Some community health centers, syringe exchange programs, and even libraries offer it for free. Ask for it by name-no shame, no judgment. It’s a lifesaving tool, not a sign of failure.
What should I do if I suspect someone is overdosing?
Call emergency services immediately. Then, if you have naloxone, administer it. Try to keep the person awake and breathing. Lay them on their side to prevent choking. Don’t wait for symptoms to get worse. Overdose can happen fast. Acting quickly saves lives.

Man, I read this and just felt like someone finally put into words what I’ve been screaming into the void for years. I’ve lost friends to this silent combo of pills and booze, and no one ever saw it coming because ‘it’s just a little Xanax’ or ‘it’s just a glass of wine.’
It’s not just about the drugs-it’s about the shame. People don’t admit to mixing because they think they’re weak, not because they’re lying. We need more spaces where asking ‘Did you take anything else?’ doesn’t feel like an interrogation.
I carry naloxone in my wallet. Not because I use, but because I know people who do. And if I can be the one who doesn’t look away, maybe someone lives to see another sunrise.
Stop judging. Start asking. It’s that simple.
Oh wow. Another ‘you’re all just lazy and don’t know what you’re doing’ lecture from the medical industrial complex. Let me guess-the next article will be ‘How to Stop Being a Drug User by Following 7 Simple Steps From a PhD Who’s Never Held a Needle.’
Here’s the truth: people use drugs because life hurts. Not because they’re stupid. Not because they didn’t read your 12-point checklist. And no, naloxone isn’t a magic fix-it’s a bandage on a bullet wound.
Meanwhile, the real killers? Poverty. Trauma. The fact that your ‘safe’ prescription opioids were handed out like candy while your neighbor got a felony for having a joint.
Fix the system. Not the users.
Overdose deaths up. Fentanyl everywhere. Mixing opioids with benzos = 10x risk. Alcohol + opioids = 67% more respiratory depression. 58% underreport benzos. 68% never asked about alcohol. CDC ORT. Beers Criteria. FDA checker. MedlinePlus. Naloxone available without prescription. 73% of dangerous interactions involve street names. SAMHSA survey showed higher disclosure with visual cards. 78% of fentanyl interactions missed by digital tools. 63% of hospitals now ask about non-prescribed substances. 17% of syringe programs have pharmacists. 88% accurate self-check tool. 10,000+ substances covered. 1,200+ drugs in FDA tool. All 50 states allow naloxone access. All facts. No fluff. No emotion. Just data.
I’ve worked in ER for 15 years. I’ve seen the same pattern over and over. Someone comes in, blue, not breathing. We give naloxone. They wake up. We ask, ‘What did you take?’ They say, ‘Just my pain pills.’ Then, after they’re stable, quietly: ‘...and the Xanax I took last night.’
It’s never about lying. It’s about fear. Fear of being judged. Fear of losing custody. Fear of being labeled an addict.
So I changed how I ask. Now I say, ‘A lot of people mix their meds with something else-sleep aids, alcohol, even weed. Did you do that?’
Almost always, they tell me. Not because I’m smart. Because I didn’t make them feel like a criminal.
It is, without a doubt, an incontrovertible fact that the confluence of central nervous system depressants constitutes a perilous pharmacological synergy, the magnitude of which is not adequately apprehended by the lay populace. The epistemological lacuna regarding the classification of substances as ‘medications’ engenders a perilous cognitive dissonance, wherein benzodiazepines and alcohol are erroneously demoted to the category of ‘non-medical’ consumption. This semantic misalignment, rooted in sociocultural norms rather than pharmacological reality, necessitates a paradigmatic recalibration in clinical discourse and public health messaging. The imperative is not merely to inform, but to reframe.
My brother died last year from mixing his oxycodone with Ambien. He didn’t even know it was dangerous. He thought Ambien was just for sleep. I’ve been crying every day since. I just wish someone had told him. I wish someone had told me. I wish I had asked him. I wish I had noticed he was always tired. I wish I had noticed he stopped laughing. I wish I had known about naloxone. I wish I had known how to talk to him without screaming. I wish I had known that ‘just one pill’ could kill. I wish I had known that he wasn’t weak-he was scared. I wish I had known that he loved me. I wish I had known that he didn’t want to die. I wish I had known.
Let us not confuse the symptoms of systemic failure with the pathology of the individual. The West, in its infinite wisdom, has commodified suffering, packaged it as ‘addiction,’ and sold it back to the masses as a moral failing. The real tragedy is not the mixing of substances-it is the absence of meaning, of dignity, of community. In India, we have a word: ‘Dukh.’ Suffering. We do not treat dukh with checklists. We sit with it. We hold space. We do not hand out naloxone like candy-we hold hands until the breath returns.
Perhaps the answer is not more tools, but more presence.
Just wanted to say this post saved my life. I was mixing my pain meds with sleep aids because I couldn’t sleep and didn’t think it mattered. I read the part about ‘anything not prescribed’ and realized I’d been doing it for years. I went to my pharmacist yesterday and asked for a full check. She found three dangerous combos I didn’t even know about. She gave me naloxone. No judgment. Just help.
Thank you for writing this. I’m not alone anymore.
There’s a quiet revolution happening in harm reduction-and it’s not about drugs. It’s about dignity. When you stop asking ‘Why are you doing this?’ and start asking ‘What do you need?’ everything changes.
I’ve trained outreach workers in Mumbai using picture cards instead of medical jargon. One guy said, ‘You showed me a picture of a blue pill and asked if I took it. I said yes. Then you asked if I wanted to live. I cried. I didn’t know anyone cared enough to ask.’
It’s not about knowing every drug interaction. It’s about knowing someone sees you. And that’s the first step to survival.
Let’s be real. Most of these people are just lazy. If you can’t read a simple warning label or Google ‘does Xanax kill you with opioids,’ then you shouldn’t be allowed near a pharmacy. Naloxone isn’t a safety net-it’s an enabler. You don’t save people from themselves by handing them pills. You save them by making them face the consequences.
Also, ‘street names’? That’s just code for ‘I don’t want to say the real word.’ Stop coddling addicts. Start holding them accountable.
Just got naloxone from my local pharmacy. No ID, no questions. They handed it to me with a smile and said, ‘You never know when you’ll need it.’ 🙏
Also, I keep one in my car. One in my backpack. One in my partner’s purse. Just in case. No shame. Just love.
@5317 - I get it. You think accountability means punishment. But accountability without compassion is just cruelty.
I’ve been clean for 8 years. I didn’t get there because someone yelled at me. I got there because someone sat with me in silence and said, ‘You matter.’
Don’t confuse your anger with morality. The people who die aren’t the ones who didn’t try. They’re the ones who were never given a reason to believe they could.