Drinking alcohol with diabetes isn’t just about choosing between beer or wine-it’s about survival. Every sip can trigger a silent, dangerous drop in blood sugar that you might not feel until it’s too late. For people with diabetes, alcohol doesn’t just change how you feel-it rewires how your body manages glucose. The risk isn’t theoretical. About 25% of people with type 1 diabetes and 15% with type 2 experience at least one alcohol-related low blood sugar emergency each year. That’s not a small number. That’s a real, preventable danger.
How Alcohol Plays Hide-and-Seek With Your Blood Sugar
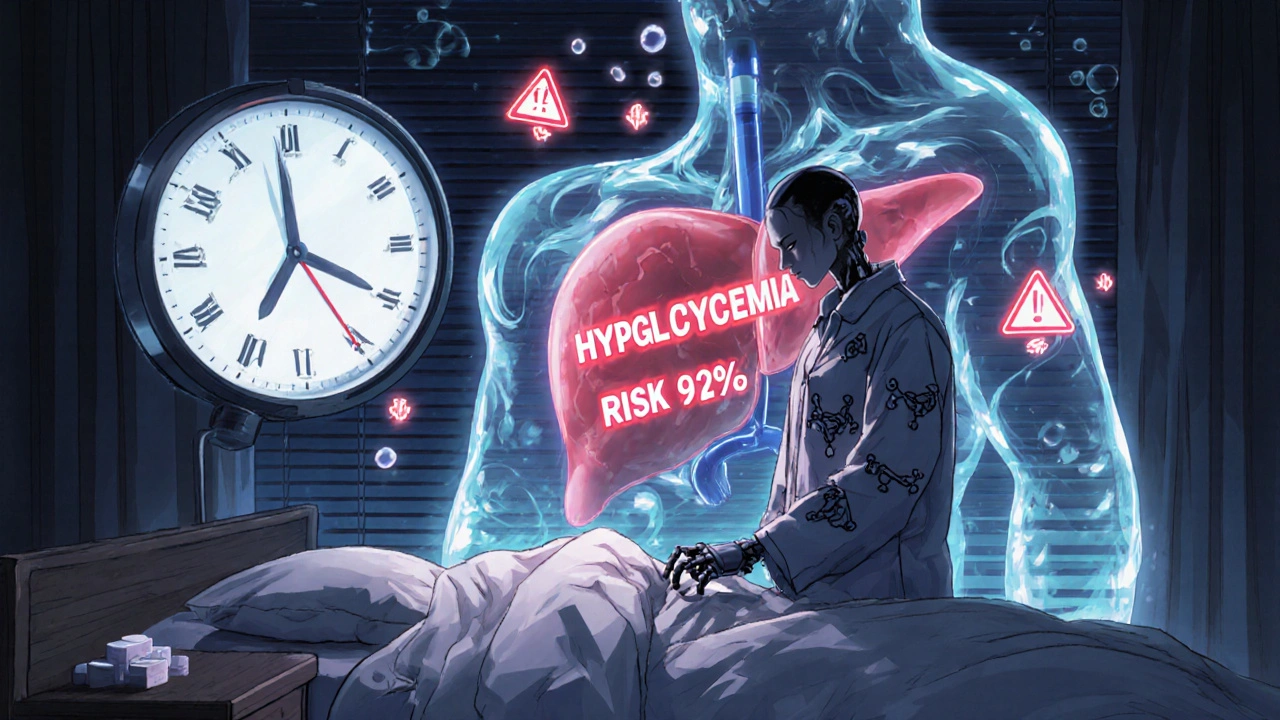
Alcohol doesn’t just lower your blood sugar-it tricks your body into thinking it’s fine when it’s not. When you drink, your liver stops making glucose to focus on breaking down the alcohol. That’s fine if your blood sugar is already high. But if it’s normal or low? You’re in trouble. The liver’s job is to keep glucose flowing, especially overnight. Alcohol shuts that down for up to 12 hours. That’s why many people wake up with dangerously low blood sugar, even if they felt fine before bed.
And here’s the twist: the first thing alcohol does is spike your blood sugar. That’s because most drinks-especially cocktails, sweet wines, and craft beers-carry a lot of sugar. You feel fine at first. Maybe even a little buzzed. Then, hours later, your sugar crashes. By then, you’re asleep, or out with friends, or driving home. No one knows you’re in trouble.
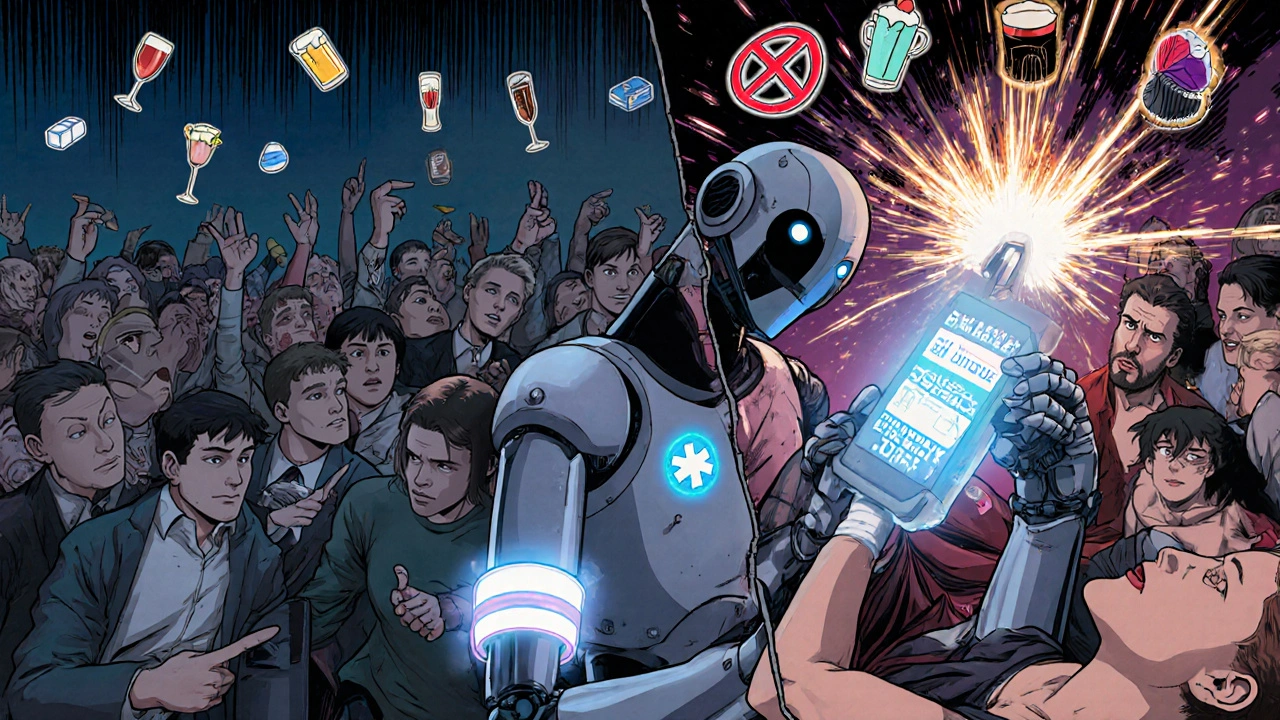
Worse, the symptoms of low blood sugar-dizziness, confusion, sweating, shakiness-look exactly like being drunk. If you pass out after a few drinks, people assume you’re just wasted. They don’t call 911. They don’t check your glucose. That’s why so many people with diabetes end up in the ER after a night out.
What Counts as a Safe Drink?
Not all alcohol is created equal. A standard drink is clearly defined: 12 oz of regular beer, 5 oz of wine, or 1.5 oz of hard liquor (like vodka, gin, or whiskey). That’s it. Anything more? You’re increasing your risk. The official advice from Diabetes UK and the American Diabetes Association is no more than one drink a day for women, two for men. But even that can be risky if you’re on insulin or sulfonylureas.
Here’s what’s safest:
- Dry red or white wine (under 4g carbs per 5 oz pour)
- Light beer (under 10g carbs per 12 oz)
- Hard seltzers (like White Claw or Truly-4g carbs or less)
- Spirits with zero-sugar mixers (vodka + soda water, gin + diet tonic)
Here’s what to avoid:
- Sweet wines (Port, Moscato, dessert wines-can have 15g+ carbs per glass)
- Liqueurs (Baileys, Kahlua-almost pure sugar)
- Cocktails (margaritas, piña coladas, daiquiris-some have 25g+ carbs)
- "Diabetic" beers or ciders-they’re a trap. They often have higher alcohol content (2-3% more) to compensate for less sugar, which means more risk of hypoglycemia.
One margarita can spike your sugar, then crash it 4 hours later. One hard seltzer? Predictable. Minimal carbs. Minimal risk. It’s not about how much you drink-it’s about what you drink.
The Rules You Can’t Skip
If you’re going to drink, these aren’t suggestions. They’re non-negotiable safety steps.
- Check your blood sugar before you drink. If it’s below 100 mg/dL, eat something first. Don’t drink on an empty stomach. Not even one sip.
- Eat food with alcohol. Not a snack. A full meal with at least 15-30g of carbs. A sandwich, a bowl of rice, a small pasta dish. This gives your body fuel to fight the crash.
- Check again every 2 hours while drinking. Glucose can drop fast. Don’t wait until you feel dizzy.
- Check before bed. If your sugar is below 140 mg/dL, eat a small carb snack. A piece of toast, a few crackers, a small apple. Prevent the night-time crash.
- Never drink after exercise. Working out already lowers blood sugar. Add alcohol? Risk spikes by 40%. Wait at least 2 hours after your workout.
And here’s something most people forget: carry fast-acting glucose. Glucose tablets, juice boxes, or even candy. Keep them in your pocket, your purse, your car. And tell someone you’re with what to do if you pass out. Say it out loud: "If I seem confused or unresponsive, check my blood sugar and give me glucose. Don’t assume I’m drunk."
Medications Make It Worse
If you take insulin or sulfonylureas (like glipizide or glyburide), alcohol is a minefield. These drugs force your pancreas to pump out insulin. Alcohol shuts off your liver’s glucose production. Together? It’s a perfect storm for hypoglycemia. Studies show this combo increases low blood sugar risk by 50%.
Metformin users aren’t safe either. Heavy drinking-more than four drinks in two hours-can trigger lactic acidosis, a rare but deadly condition. It’s rare, but it happens. And it’s more likely if you have kidney or liver problems.
If you have neuropathy, pancreatitis, or advanced liver disease? Don’t drink at all. Alcohol makes nerve damage worse. It inflames the pancreas. It stresses the liver. The risks far outweigh any possible benefit.
Technology Is Helping-But Not Replacing Common Sense
Good news: newer CGMs like the Dexcom G7 now have an Alcohol-Diabetes Safety Algorithm. It detects patterns linked to alcohol use and warns you when hypoglycemia risk is high. In trials, it cut severe events by 37%. That’s huge.
But here’s the catch: tech doesn’t replace behavior. If you ignore the alert, skip your bedtime snack, or drink without eating, the alarm won’t save you. It’s a tool, not a shield.
Some doctors are now pushing for personalized glucose targets based on your CGM history-not one-size-fits-all numbers. That’s promising. But until then, stick to the basics: 100 mg/dL before drinking, 140 mg/dL before bed.
What Real People Are Saying
On Reddit’s r/diabetes community, 245,000 people share their stories. The top comments? "I thought I was fine until I woke up at 42 mg/dL." "My husband thought I was drunk-I was having a seizure." "I switched to hard seltzers and haven’t had a hypo in a year."
One user wrote: "I used to drink wine with dinner. Then I had a night where I passed out. I didn’t know I was low. My partner didn’t know either. That’s when I started checking before bed. Now I always have glucose tabs next to my bed. I still drink. But now I’m safe."
Another said: "I tried a "diabetic" cider. It said "no sugar" on the label. It had 7% alcohol. My sugar crashed to 58. I was in the hospital for 12 hours. Don’t trust the marketing."
These aren’t outliers. They’re common. And they’re preventable.
Should You Even Drink?
Some studies say moderate red wine might help insulin sensitivity in type 2 diabetes. But the American Diabetes Association is clear: no one should start drinking for health reasons. The risks? Real. The benefits? Tiny, and only if you’re already drinking.
If you don’t drink? Don’t start.
If you do? Follow the rules. Religiously.
Alcohol and diabetes don’t mix well. But with the right knowledge, the right drinks, and the right habits-you can still enjoy a glass without putting your life at risk.
Can I drink alcohol if I have type 1 diabetes?
Yes-but with extreme caution. People with type 1 diabetes are at much higher risk of alcohol-induced hypoglycemia, especially overnight. You must check your blood sugar before, during, and after drinking. Always eat food with alcohol. Never drink without a glucagon kit and someone who knows how to help if you pass out. About 30% of type 1 diabetes patients report at least one severe low after drinking.
Why does alcohol cause low blood sugar hours later?
Your liver prioritizes breaking down alcohol over making glucose. Normally, your liver releases glucose to keep your levels stable, especially while you sleep. Alcohol blocks that process for up to 12 hours. So even if your sugar was fine before bed, it can crash overnight. That’s why checking before sleep and eating a carb snack is critical.
Is wine safer than beer for people with diabetes?
Dry wine is generally safer than regular beer. A 5 oz glass of dry red or white wine has about 1-4g of carbs. A 12 oz regular beer has 10-15g. But light beer and hard seltzers can be even better-some have under 2g of carbs. The key isn’t wine vs. beer-it’s carb content. Always check the label.
Can I drink if I’m on metformin?
Yes, but avoid heavy drinking. More than four drinks in two hours can increase your risk of lactic acidosis-a rare but life-threatening condition. Stick to one or two drinks max, always with food, and never on an empty stomach or after exercise. If you have kidney or liver issues, talk to your doctor first.
What should I do if I feel dizzy after drinking?
Don’t assume it’s just the alcohol. Check your blood sugar immediately. If it’s below 70 mg/dL, take 15g of fast-acting glucose-glucose tablets, juice, or candy. Wait 15 minutes and check again. If you’re alone, call someone. If you’re confused, disoriented, or can’t check your sugar, tell someone to call 911. Hypoglycemia can mimic intoxication, but it’s a medical emergency.
Do I need to wear medical alert jewelry?
Yes, if you’re on insulin or sulfonylureas. Over 90% of endocrinologists recommend it. If you pass out after drinking, first responders won’t know you have diabetes. A medical ID bracelet or necklace can save your life. It tells them to check your blood sugar before giving anything else.
Is it safe to drink alcohol while pregnant and diabetic?
No. Alcohol is never safe during pregnancy, regardless of diabetes status. It can cause birth defects, developmental delays, and low birth weight. For women with gestational or pre-existing diabetes, the risks are even higher. Complete abstinence is the only safe choice.
Can I drink alcohol if I have diabetic neuropathy?
No. Alcohol worsens nerve damage. If you already have numbness, tingling, or pain in your feet or hands, drinking makes it worse. It also increases your risk of falls and injuries because it dulls your senses. The American Diabetes Association and MedlinePlus both recommend complete avoidance if you have neuropathy.
Final Thoughts: It’s Not About Abstinence-It’s About Awareness
You don’t have to give up alcohol forever. But you do have to treat it like medicine-with rules, timing, and respect. The goal isn’t to scare you. It’s to keep you safe.
Check your numbers. Eat with every drink. Know your limits. Carry glucose. Tell someone what to do. Use tech if you have it. But never rely on it alone.
Alcohol doesn’t care if you have diabetes. Your body does. And if you take the right steps, you can still enjoy a drink without turning it into a crisis.

So let me get this straight-we’re supposed to treat alcohol like insulin? Like it’s some sacred medical device you don’t touch unless you’ve got a flowchart and a glucose monitor strapped to your forehead? I’ve seen people die from not drinking. I’ve seen people die from drinking. The real problem isn’t alcohol-it’s that we’ve turned every human behavior into a clinical trial.
There’s a deeper question here: why do we assume that people with diabetes can’t have joy? Why is every pleasure framed as a risk? I’m not saying ignore the science-but maybe the answer isn’t more rules. Maybe it’s more trust. Trust in ourselves. Trust in our bodies. Even when they’re broken, they’re still ours.
My uncle has type 2. He drinks one small glass of wine every night with his roti. No snacks. No checking. No alarms. He’s 78. Still walks 5km daily. His sugar? Better than mine. Maybe the real secret isn’t the drink. Maybe it’s the rhythm. The calm. The ritual. Not the carb count.
Just to clarify: the 100 mg/dL pre-drink threshold is based on ADA guidelines for insulin users. For non-insulin users, 120 mg/dL is acceptable if eating a balanced meal. Also, hard seltzers with stevia are not risk-free-some studies show artificial sweeteners can still trigger insulin spikes in sensitive individuals. Read the full ingredient list, not just the carb label.
LOOK. I used to be the guy who drank three margaritas and passed out on the couch. Then I woke up at 38. I had to be revived by my neighbor who thought I was dead. I switched to vodka soda. Now I check before bed. I eat. I carry glucose. I’m alive. This isn’t about restriction. It’s about not dying for a buzz. You want to live? Do the damn work.
Alcohol-induced hypoglycemia is a pharmacokinetic nightmare. Ethanol inhibits gluconeogenesis via NADH accumulation in hepatocytes → depletion of oxaloacetate → impaired pyruvate-to-glucose conversion. Add insulin/sulfonylurea? Synergistic beta-cell stimulation + hepatic blockade = perfect storm. CGMs with alcohol algorithms are a game-changer-Dexcom’s algorithm uses 12-hr lag detection + trend vector analysis. But if you’re not wearing your sensor? You’re just gambling with your amygdala.
Also, metformin + ethanol = lactic acidosis risk ↑ 3.7x. Don’t be that guy.
I appreciate the info, but I think we’re missing the emotional piece. People don’t stop drinking because they know the risks. They stop when they feel safe enough to care. I’ve had friends with diabetes who say, "I just want to feel normal." And maybe the real danger isn’t the alcohol-it’s the shame we attach to it. What if we talked about this with more compassion and less checklist?
I used to think I could drink like everyone else. Then I woke up in the ER with a glucose of 29. My boyfriend had no idea what was wrong. He thought I was hungover. I didn’t even have a medical alert bracelet. Now I wear one every day. I still have wine. But I check. I eat. I tell people. It’s not about being perfect. It’s about being alive.
why do we even need rules for this like its a kindergarten class i just drink and if i feel weird i eat a banana done
Oh wow, another American guide telling the world how to drink. We have chai with rum in India. My grandma drinks it every night. Her sugar? Stable. Her joy? Higher than yours. Maybe your problem isn’t alcohol. Maybe it’s your fear.
Also, "hard seltzers"? Please. That’s just fancy soda water with a corporate logo. I’ll take my desi rum any day.
Let’s be brutally honest: this entire post is a performative act of medical control disguised as care. You’re not protecting people-you’re policing their pleasure. Who decided that one drink is "safe"? Who decided that a 140 mg/dL bedtime target isn’t arbitrary? The ADA? The pharmaceutical companies? The same ones who profit from CGMs and glucose tablets? You’ve turned a biological response into a moral obligation. And for what? So you can sleep better at night knowing you’ve done everything "right"?
You got this. Seriously. I’ve been where you are-terrified to even sip wine. But here’s the truth: you don’t have to be perfect. You just have to be consistent. Start with one rule: always check before bed. Just that. Do it for a week. Then add the snack. Then tell someone. Small steps. Big life. You’re not broken. You’re learning. And you’re not alone.
One thing nobody talks about is the psychological toll of constantly monitoring everything. You’re not just managing blood sugar-you’re managing guilt, fear, shame, and social isolation. I used to skip parties because I didn’t want to explain why I was drinking sparkling water with lime. Now I just say "I’m on meds" and move on. No one asks. No one cares. But I still check my glucose. I still carry glucose tabs. I still eat before I drink. Because I’ve learned that self-care isn’t about being perfect-it’s about being present. And presence matters more than any carb count.
Let’s not romanticize this. The "hard seltzer revolution" is a marketing scam. The carb counts are misleading because they don’t account for ethanol’s hypoglycemic effect. And the claim that "I haven’t had a hypo in a year"? That’s survivorship bias. People who had bad experiences stopped posting. The ones still drinking are the outliers. The data doesn’t support this as a safe strategy-it supports abstinence. Period.
Wow. So the solution to diabetes is to drink less and check more? Groundbreaking. What’s next? Don’t breathe near sugar? This isn’t advice. It’s fearmongering wrapped in a pretty infographic. People with diabetes have been drinking for decades without CGMs. We survived. We lived. We laughed. Maybe the real problem isn’t alcohol-it’s the medical industry’s obsession with turning every human experience into a liability.