Multiple System Atrophy (MSA) isn’t just another form of Parkinson’s disease. It’s a faster, crueler, and far less understood neurodegenerative disorder that steals movement, balance, and even basic bodily functions-often before people realize what’s happening. While Parkinson’s affects about 1 million Americans, MSA strikes only 15,000 to 50,000 people in the U.S., making it rare but devastating. The most common form, MSA-P (parkinsonian type), makes up 65-70% of cases and mimics Parkinson’s at first: slow movement, stiff muscles, shaky hands. But the similarities end there.
What Makes MSA-P Different from Parkinson’s?
At first glance, MSA-P looks like Parkinson’s. People stumble, move slowly, speak softly, and their faces lose expression. But the differences are critical. In Parkinson’s, tremors usually happen at rest-like when the hand is resting on a lap. In MSA-P, tremors are more likely to appear when reaching for something, and they’re jerky, not rhythmic. About 60% of MSA-P patients develop these tremors, but they don’t respond the way Parkinson’s tremors do.
The biggest red flag? Levodopa. It’s the gold-standard treatment for Parkinson’s. For MSA-P, it barely works. Only 15-30% of patients get any real benefit, and even then, it lasts maybe a year or two before fading. That’s not just a minor setback-it’s a major clue that something more aggressive is happening in the brain.
MSA doesn’t just attack the substantia nigra, where Parkinson’s starts. It spreads to the basal ganglia, brainstem, and cerebellum. The hallmark sign? Glial cytoplasmic inclusions filled with alpha-synuclein protein. These abnormal clumps destroy nerve cells across multiple systems, not just one. That’s why symptoms don’t stay limited to movement.
The Silent Killer: Autonomic Dysfunction
What makes MSA-P so dangerous isn’t just the shaking or stiffness-it’s what happens when your body can’t regulate itself. Autonomic failure isn’t a side effect; it’s a core feature. Up to 90% of patients develop orthostatic hypotension: a dangerous drop in blood pressure when standing. This isn’t just dizziness. It’s fainting, falls, head injuries, and sometimes sudden death.
Urinary problems hit 85-90% of people. It starts with urgency, then frequency, then complete incontinence. For men, erectile dysfunction isn’t a late-stage issue-it’s often the first symptom, appearing years before any trouble walking. One patient shared on a support forum that he went to the doctor for trouble peeing at age 48. Three years later, he couldn’t stand without help.
Sleep is another battleground. Eighty to ninety percent of MSA-P patients act out their dreams-kicking, yelling, even jumping out of bed. This is REM sleep behavior disorder, and it’s one of the earliest warning signs. Add in sleep apnea (60-70% of cases), and you’ve got someone exhausted before the day even begins.
Temperature control vanishes. Half of patients stop sweating in patches-no sweat on the back, but soaked armpits. That means overheating in mild weather, or freezing when others are comfortable. It’s a body that’s lost its thermostat.
How Fast Does It Progress?
Time is the enemy in MSA-P. Unlike Parkinson’s, where people can live for decades with manageable symptoms, MSA moves fast. Within 1-2 years of symptoms starting, 85% of patients have already fallen at least once. By 3.5 years, most need a cane or walker. By 5.3 years, they’re in a wheelchair. Five years after diagnosis, half have lost most of their motor skills.
The median survival? Just 6 to 10 years from symptom onset. Only 52-68% are alive at the five-year mark. By ten years, that number drops to 9-23%. Those who respond poorly to levodopa live even shorter lives-around 6.2 years on average. Those who get some benefit? Maybe 9.8 years. But even that’s a grim hope.
The leading causes of death? Respiratory infections (45%), sudden cardiac events (20%), and choking from swallowing problems (15%). The brain doesn’t just stop controlling movement-it stops controlling breathing, heart rhythm, and the reflex to clear the throat. One patient on a support group wrote: “I’m 55. My neurologist said I won’t see 65. I’m trying to make every day count.”
Diagnosis: The Long Wait for an Answer
Getting diagnosed with MSA-P is a nightmare. Early on, it looks like Parkinson’s. Even experienced neurologists get it wrong. Diagnostic accuracy only hits 85-90% after 3-5 years. That’s years of misdiagnosis, wrong treatments, and wasted time.
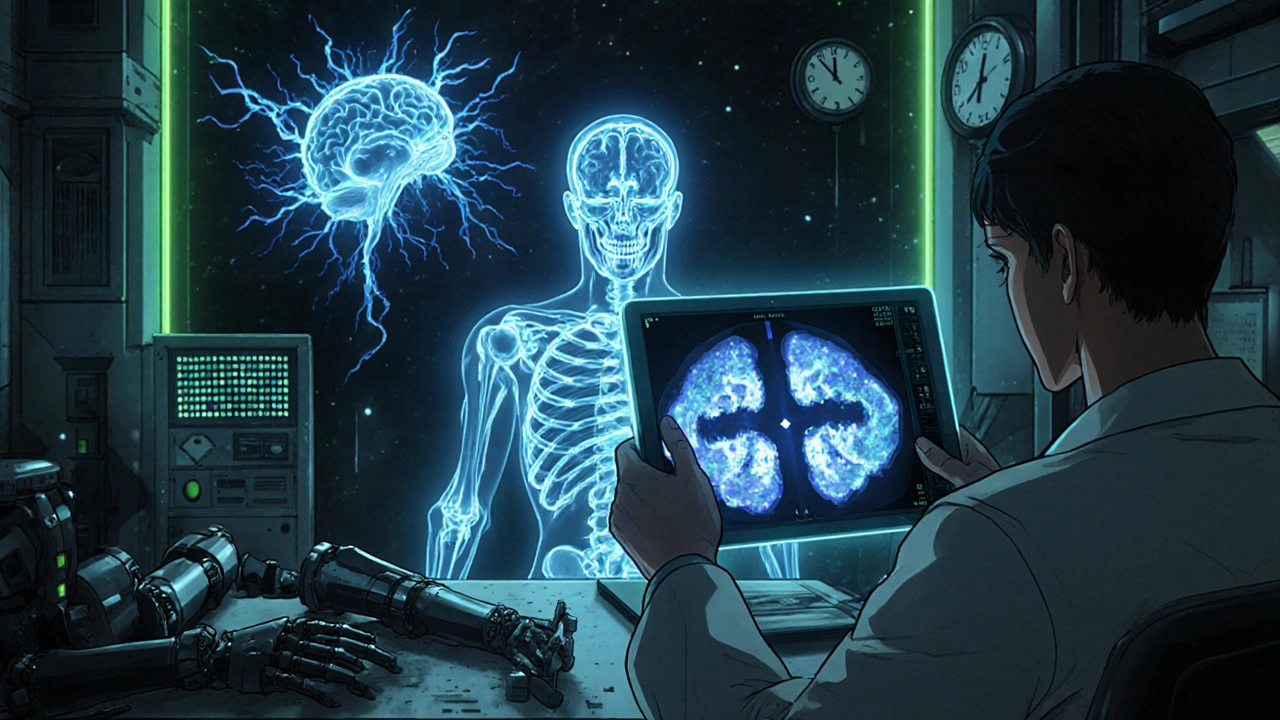
Key clues? Autonomic symptoms showing up within three years of movement problems. That’s the strongest predictor. MRI scans can help: the “hot cross bun” sign in the brainstem (seen in 50-80% of MSA-C cases) or shrinking of the putamen (a part of the basal ganglia). Blood tests for neurofilament light chain-a protein that leaks when nerves die-are rising in use. Levels in MSA patients are 3-5 times higher than normal.
Right now, diagnosis relies on a mix of clinical signs, imaging, and autonomic testing. But researchers are working on a biomarker panel that could cut diagnosis time to under a year. A major study, NCT04567615, is testing this approach and should release results in early 2024. For families waiting for answers, that can’t come soon enough.
Treatment: Managing Symptoms, Not Stopping the Disease
There’s no cure. No drug stops MSA-P from progressing. Treatment is about keeping people as safe and comfortable as possible for as long as possible.
For low blood pressure: fludrocortisone, midodrine, or droxidopa. These help keep blood pressure up when standing. But they don’t fix the root problem-they just patch the leak.
Levodopa is still tried, often at high doses (up to 1,000 mg/day). But doctors warn: if there’s no improvement after 3-6 months, stop. It’s not worth the side effects.
Physical therapy helps maintain mobility. Speech therapy tackles slurred speech and swallowing risks. Urologists manage bladder issues with catheters or medications. Sleep specialists treat REM behavior disorder with melatonin or clonazepam.
And yet-despite all this, quality of life plummets. A 2021 survey of 327 MSA patients found 78% rated their quality of life as “poor” or “very poor” within four years of diagnosis. For Parkinson’s patients at the same stage? Only 35% felt that way.
What’s on the Horizon?
Research is painfully slow. As of late 2023, there were only three active clinical trials worldwide targeting MSA’s root cause. Most focus on stopping alpha-synuclein buildup. The PASADENA trial tested an immunotherapy drug. It showed a tiny 1.2-point slower decline on a rating scale over 18 months-statistically significant, but clinically meaningless to most patients.
Dr. Lucy Norcliffe-Kaufmann, a leading MSA researcher, says the biggest problem isn’t treatment-it’s timing. “By the time motor symptoms appear, 50-70% of the nerve cells are already gone.” That’s why early detection is the real goal. If we could catch MSA before the tremors start, we might have a shot.
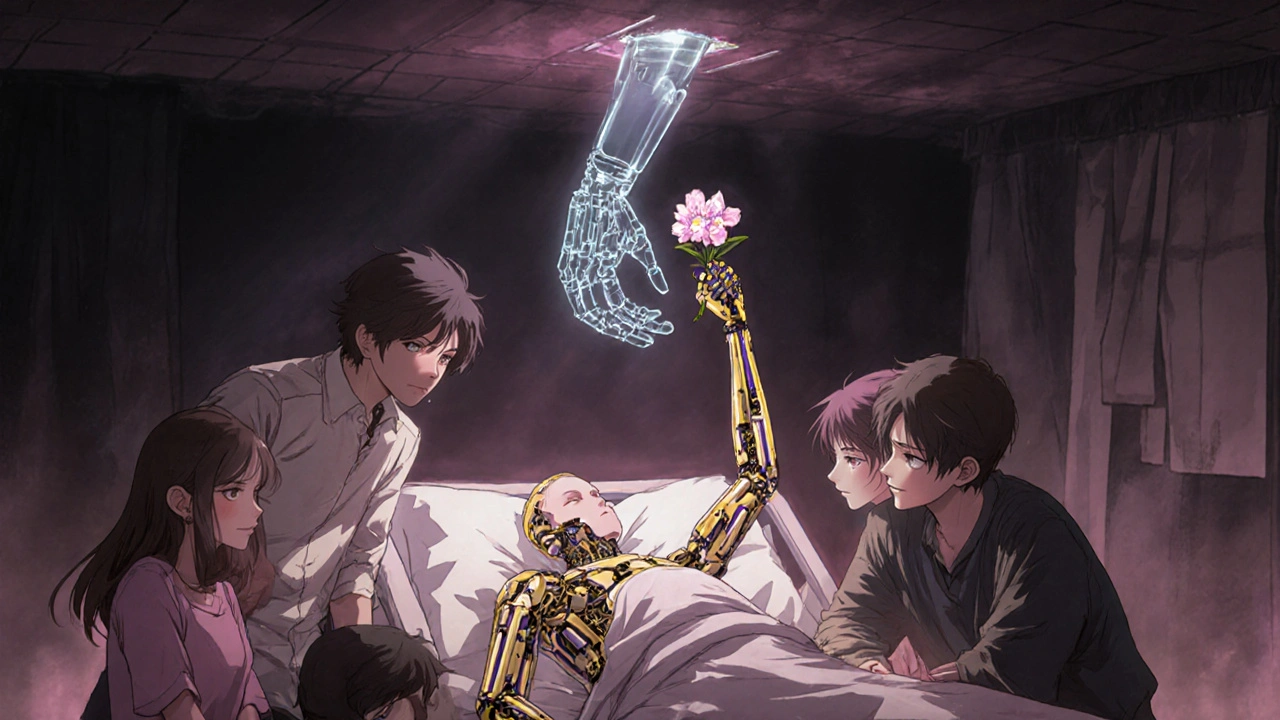
For now, the prognosis remains grim. Without a breakthrough in understanding how alpha-synuclein spreads or why nerve cells die so rapidly, median survival is unlikely to extend beyond 10 years in the next decade. Families are left with hard choices: when to get a feeding tube, when to stop driving, when to say goodbye.
MSA-P doesn’t just take your ability to walk. It takes your independence, your dignity, your future. And it does it quickly.
Is Multiple System Atrophy the same as Parkinson’s disease?
No. While MSA-P shares some symptoms with Parkinson’s-like slow movement and stiffness-it’s a different disease. MSA affects more areas of the brain, causes severe autonomic failure early on, and doesn’t respond well to levodopa. Parkinson’s progresses slowly over decades; MSA-P usually leads to severe disability within 5 years.
Can MSA be cured?
No, there is no cure for MSA. Current treatments focus on managing symptoms like low blood pressure, urinary problems, and movement issues. Research is ongoing, but no therapy has yet been shown to stop or reverse the disease.
How long do people live after being diagnosed with MSA-P?
Median survival is 6 to 10 years from symptom onset. About half of patients die within 5 years, and only 9-23% survive past 10 years. Those with poor response to levodopa tend to have shorter lifespans-around 6 years on average.
What are the early warning signs of MSA-P?
Early signs often include orthostatic hypotension (dizziness on standing), urinary incontinence, erectile dysfunction in men, and acting out dreams during sleep (REM sleep behavior disorder). These can appear years before movement problems like stiffness or shuffling gait.
Why doesn’t levodopa work well for MSA-P?
Levodopa helps replace dopamine in Parkinson’s, where dopamine-producing cells in the substantia nigra are damaged. In MSA-P, the damage is broader-nerve cells in multiple brain regions die, and the brain’s ability to use dopamine is impaired. Even if dopamine is added, the system can’t respond properly.
Is MSA-P hereditary?
No, MSA-P is not inherited. It occurs sporadically, with no known genetic cause. It doesn’t run in families, and there’s no genetic test available to predict it.
What can families do to help someone with MSA-P?
Families should focus on multidisciplinary care: physical therapy to maintain mobility, speech therapy to prevent choking, urology for bladder management, and palliative care to manage symptoms and quality of life. Early planning for feeding tubes, wheelchairs, and hospice can reduce stress later. Support groups, like the MSA Coalition, offer practical advice and emotional support.
What Comes Next?
For those living with MSA-P, the road ahead is steep. But knowledge is power. Understanding the timeline, the risks, and the options helps families make decisions before crisis hits. It’s not about fighting the disease-it’s about living as fully as possible while it’s still possible.
The next decade may bring better diagnostics-maybe even a blood test that spots MSA before symptoms start. But until then, the focus remains on comfort, safety, and dignity. Because in a disease this fast, time isn’t just measured in years-it’s measured in moments.

Levodopa barely works? That’s it. I’m done. No more false hope.
I read this whole thing and just sat there crying. Not because I have it-but because I know someone who does. The part about not sweating on your back but drenching your armpits? That’s my uncle. He never told anyone. Just kept wearing the same shirt for days. No one understood. Now I do. And I hate that I do.
This isn’t just medical. It’s a slow erasure of personhood. They take your bladder, your sleep, your voice, your balance-and then act surprised when you stop going out. No one talks about the loneliness. The way your friends slowly stop calling because they don’t know what to say. And you’re too tired to explain.
I’m from India and I’ve seen patients with MSA in our neurology ward-rare, yes, but devastatingly clear when you see it. The autonomic failure is the real monster. One patient, 52, kept fainting during dialysis because his BP dropped too fast. We had to adjust his meds, his diet, his posture-everything. But the real tragedy? He was diagnosed after 2 years of being told he had Parkinson’s. By then, his cerebellum was already collapsing. No cure, no trial nearby, no money for specialized care. Just a wife who learned how to catheterize him in the kitchen. This disease doesn’t care about borders or insurance. It just takes.
So if REM sleep disorder shows up years before tremors… why aren’t we screening people for it? Like, if you’re 45 and you’re punching your pillow every night, shouldn’t someone run a blood test or an MRI? Why wait for the fall? Why wait for the incontinence? This feels like we’re playing whack-a-mole with symptoms instead of stopping the root cause.
Actually, the alpha-synuclein pathology is shared with Lewy body dementia and Parkinson’s-so it’s not unique. What makes MSA distinct is the glial cytoplasmic inclusions, not just the protein. And the putaminal atrophy on MRI is more specific than the hot cross bun sign, which is more common in MSA-C. Also, neurofilament light chain isn’t FDA-approved for MSA diagnosis yet-it’s still research-grade. Don’t get misled by headlines. The real diagnostic gold standard remains clinical criteria from the Second Consensus Statement, 2008. You need autonomic failure + either parkinsonism or cerebellar signs. Everything else is supportive.
Let’s be brutally honest: we’re not fighting a disease-we’re fighting entropy. The brain is a symphony of electrical and chemical signals, and MSA? It’s the conductor dropping the baton… then setting the entire orchestra on fire. Alpha-synuclein isn’t just misfolding-it’s *corrupting*. It’s a prion-like cascade. And we’re treating it like a vitamin deficiency. We give levodopa like it’s aspirin. We put in catheters like it’s a plumbing issue. But the system isn’t broken-it’s *unraveling*. And until we accept that we’re dealing with a systemic collapse of neural integrity-not just a dopamine shortage-we’re just rearranging deck chairs on the Titanic.
I used to think time was the enemy. Now I think it’s the illusion. MSA doesn’t steal years-it steals presence. The man who couldn’t stand? He still laughed at his granddaughter’s drawings. The woman who couldn’t swallow? She whispered poetry to her husband every night. The disease takes the body, but not the soul-unless we let it. Maybe the real breakthrough isn’t in a lab. Maybe it’s in learning how to love someone even as they fade. Not with hope for a cure… but with courage for the now.